A patient's endometrial thickness can greatly increase or decrease the success of embryonic implantation. Literature designates ideal endometrial thickness at or above 7 mm, as measured by transvaginal ultrasound. Patients whose uterine linings are thinner than that have less optimal conditions for implantation and a markedly lower chance of becoming pregnant.
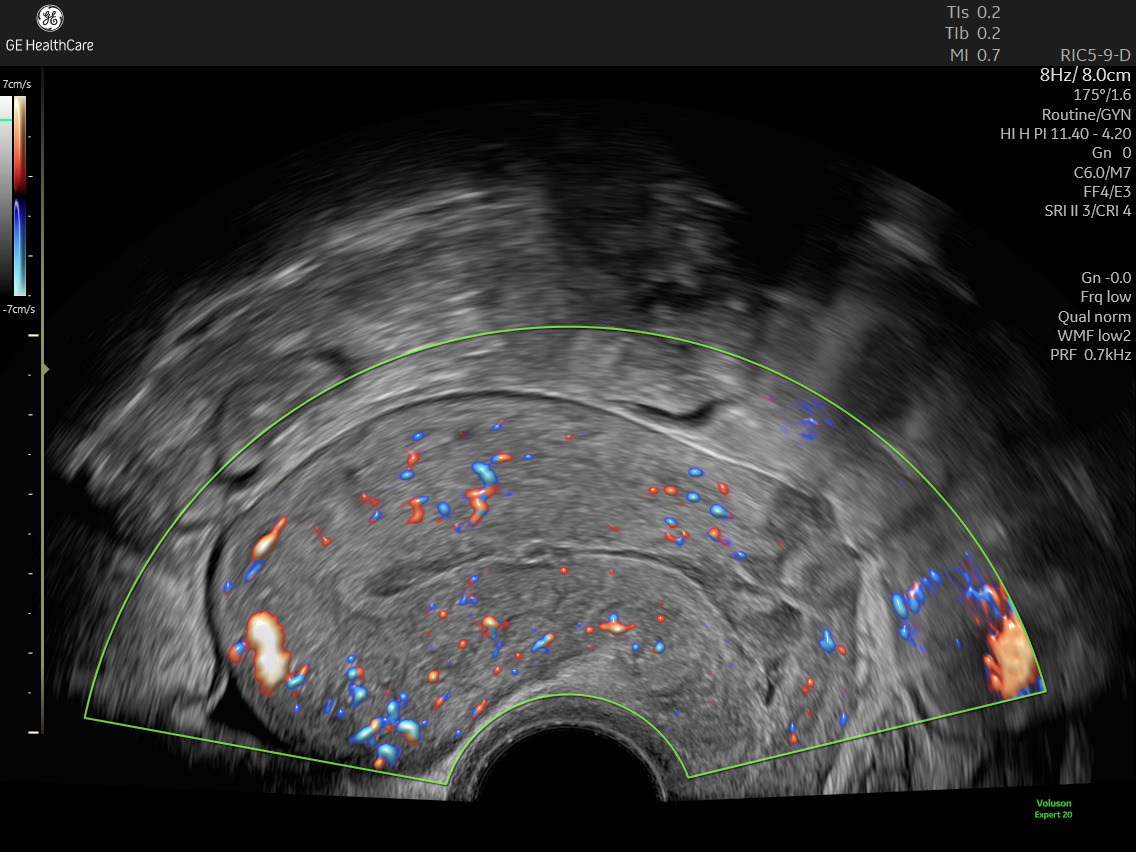
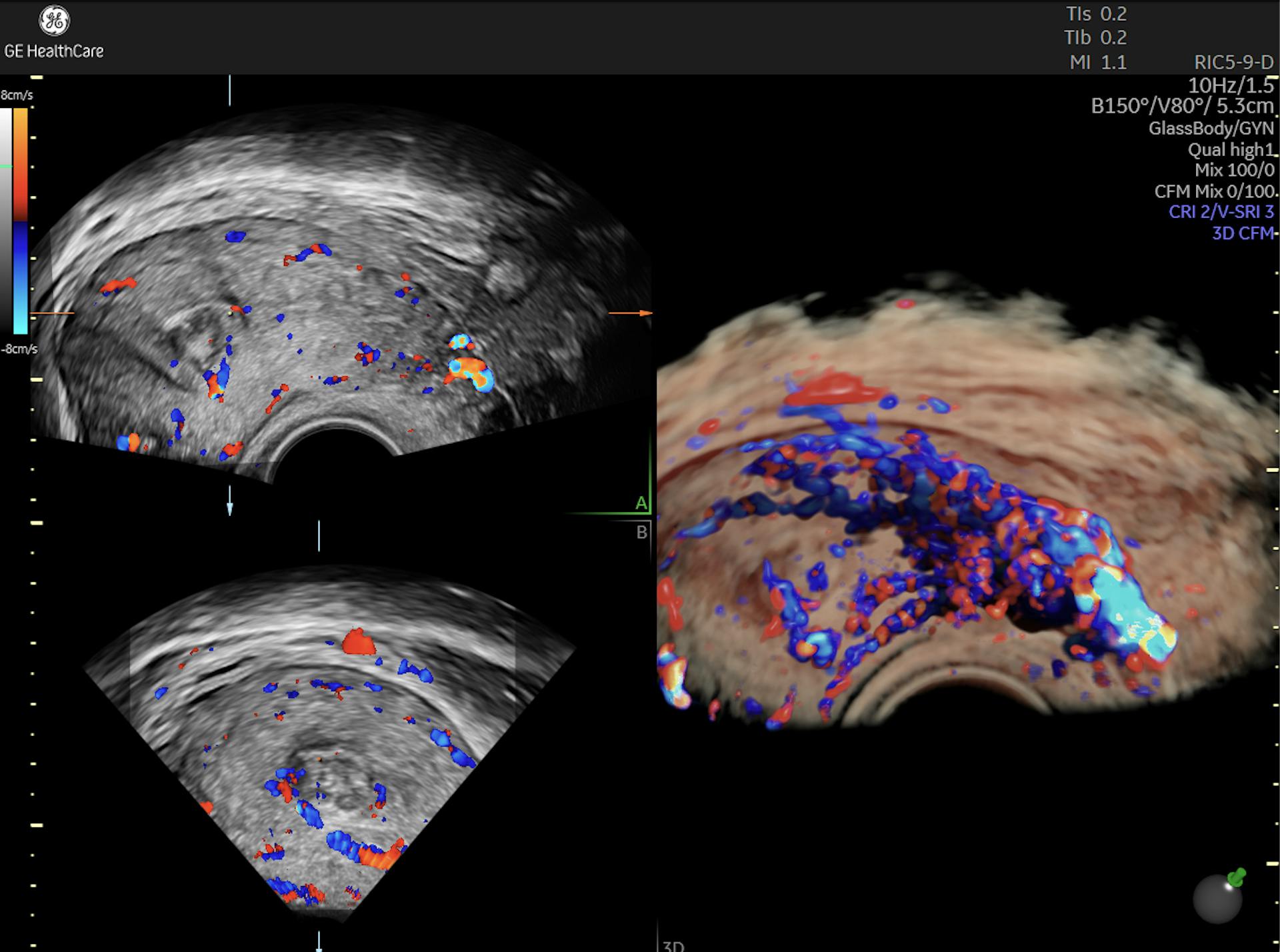
Endometrium shown on ultrasound using Radiantflow™ imaging technology
But is it possible to boost endometrial receptivity by thickening the endometrium? Recent research has explored key techniques to do exactly that. Some studies have revealed standout approaches, while others have had mixed or insufficient results.
These three methods, along with careful ultrasound monitoring, warrant consideration by practitioners as ways to help give a patient with a thinner endometrium the best chance of success.
1. Vaginal Sildenafil
Sildenafil has shown promising effects when applied as a gel or suppository to the vaginal area. Known as Viagra in its more common form, this drug has a host of other applications thanks to its impact on blood flow, including endometrial proliferation.
In an analysis of several treatments published in the Middle East Fertility Society Journal, Sildenafil was shown to measurably increase endometrial thickness. In one of the protocols studied, participants who took a 25 mg dose four times a day saw increases in endometrial thickness exceeding 9 mm and higher rates of implantation and pregnancy.
A small-scale study published in Facts, Views and Vision analyzed women who had undergone previous failures with clomiphene citrate (CC). Participants experienced increases in endometrial thickness — 9.3 mm versus 6.6 mm — when twice-daily 50 mg Sildenafil was added to their existing CC regimen.
2. Platelet-Rich Plasma Treatment
Over the past several years, platelet-rich plasma (PRP) treatments have become popular in several healthcare specialties, notably within cosmetic surgery, wound healing and orthopedics.
This procedure works by isolating the growth factor-rich PRP from blood extracted from peripheral veins and re-injecting the plasma back into patients. Supercharged with growth-boosting platelets, the blood can go straight to work in supporting cell and tissue development.
Studies have shown the reproductive success of PRP when administered via intrauterine infusion specifically for patients with a history of inadequate endometrial growth. In one pilot study among 10 patients published in JBRA Assisted Reproduction, an increase in lining thickness was universal within two days of PRP. After the second infusion, thickness exceeded 7 mm for all participants. Following implantation, five women became pregnant and four carried to term.
Another study among 22 patients published in Frontiers in Endocrinology found that while PRP increased thickness in more than half of participants, it surprisingly decreased thickness in seven patients. However, PRP still improved reproductive outcomes, which the authors posited may indicate other benefits of PRP beyond thickening alone.
3. Intrauterine G-CSF
For more than two decades, Granulocyte-colony stimulating factor (G-CSF) has been used to stimulate the production of granulocytes in patients undergoing chemotherapy.
Specific to fertility treatment, studies have demonstrated G-CSF's role in endometrial growth when administered via infusion. In one study of four patients whose linings ranged between 3 and 6.5 mm, G-CSF thickened linings to at least 7 mm within two days. All four patients became pregnant; one had an ectopic pregnancy. More recently, a meta-analysis among 683 patients published in the American Journal of Reproductive Immunology showed that G-CSF boosted thickness, pregnancy rates and implantation success while reducing the risk of cycle cancellation.
Based on these studies, clinicians may have ample opportunities to promote endometrial growth, dependent on patient needs. While research is ongoing, emerging approaches foreshadow a promising future for solutions in this area of infertility.