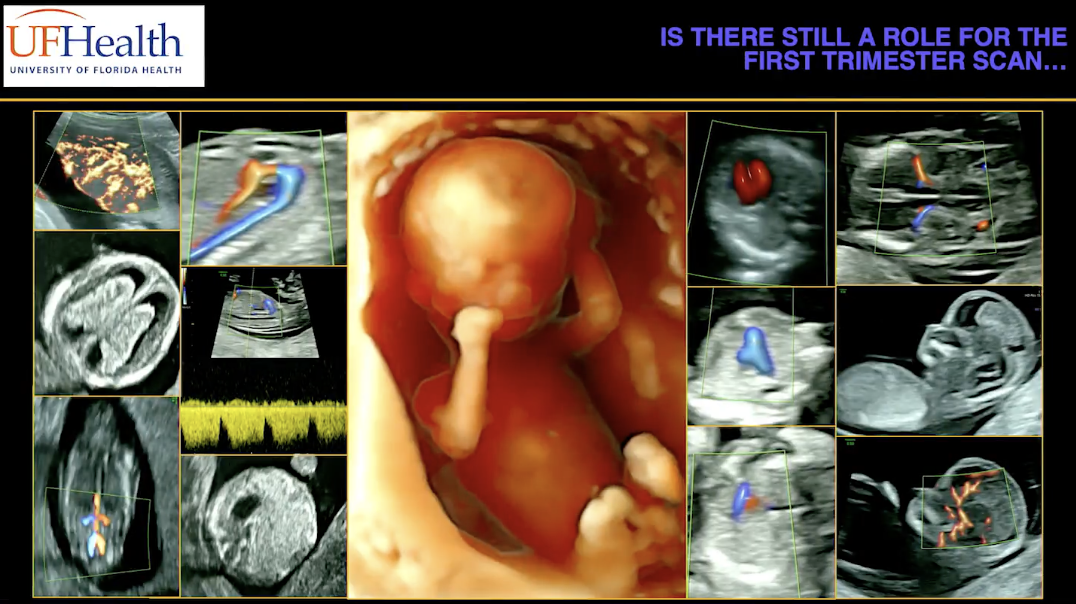
Clinicians typically employ first-trimester ultrasound to confirm pregnancy dating, determine the number of fetuses, and check the fetal heartbeat. But the first trimester can also hold important clues about the health of the fetus and whether there are any congenital malformations present.
According to Dr. Reem Abu-Rustum, an associate professor at the University of Florida and president-elect of the International Society of Ultrasound and Obstetrics and Gynecology (ISUOG), the main instigator for ultrasound in the first trimester is nuchal translucency (NT). This assessment dates back to 1866 when British physician John Langdon Down first described Down syndrome as skin that is deficient in elasticity with a small nose.

Nuchal translucency measurement taken of 12 week fetus.
In 1985, Dr. Beryl Benacerraf described the nuchal fold as a second trimester marker for Down syndrome. Seven years later, Dr. Kyprianos Nicolaides developed methods of early screening for chromosomal abnormalities by measuring nuchal translucency, revolutionizing obstetrics and gynecology. From 1992 to 2011, prior to non-invasive prenatal screening (NIPS), 70 percent of pregnancies presented for NT assessment at 11 to 14 weeks gestation.
Abu-Rustum notes that congenital malformations are almost seven times more common than chromosomal aberrations, which is why it's important not to lose access to a fetus in the first trimester. Since the introduction of NT and with advancements in technology, early ultrasound scanning has improved significantly.
"With the equipment we have today, we are able to study the developing fetus with so much detail and at much earlier points in gestation," Abu-Rustum says. "We are able to look at the vasculature, and we are able to study beyond structure, going into function."
The Importance of Detecting Abnormalities Early
Abu-Rustum notes that there are several reasons to detect abnormalities early. First, patients want to know, which gives sonographers time to do workups and discuss options with families. This counselling is especially critical because there are legal limits for terminating a pregnancy, and it is safer to do so earlier in the pregnancy.
If the patient decides to continue the pregnancy, ultrasound in the first trimester also allows sonographers to explain sudden intrauterine fetal demise and monitor the natural progression of certain conditions. Early detection can also be reassuring for patients who have already had children with abnormalities.

A fetus with Spina Bifida, clearly visualized with HDlive™ Silhouette

Acrania in first trimester visualized with HDlive™ technology
ISUOG vs. AIUM Guidelines
The ISUOG first issued guidelines for first-trimester ultrasound in 2013 and updated them in 2023. The American Institute of Ultrasound in Medicine (AIUM) issued its first-trimester practice parameters in 2020.
Both sets of guidelines have the primary goals of screening aneuploidy, establishing dating and chorionicity, and detecting structural anomalies. They also stress the importance of amnionicity in multiple gestation, as well as screening and counselling.
However, the ISUOG guidelines highlight obstetric complications more than the AIUM guidelines. There is also a slight difference in the timing of the guidelines. AIUM guidelines range from 12 weeks to 13 weeks and six days. ISUOG guidelines, on the other hand, go from 11 weeks to 14 weeks. According to Abu-Rustum, structure is the main reason for these differences.
"The further we are in gestation, the better our ability to detect structural abnormalities," she says. "If you are not using NIPS and you are using NT for aneuploidy, the earlier you are, the more sensitive NT is."
The Goals of First-Trimester Ultrasound Scanning
Abu-Rustum explains that there are several goals for performing a scan in the first trimester. The main goal is safety. It's important to determine the location of the fetus and ensure that it's a properly placed intrauterine gestation. It's also essential to determine viability and the number of fetuses.
Dating is another important component of the AIUM and ISUOG guidelines, especially in the case of twins, Abu-Rustum notes. Discordance in the crown rump length (CRL) and nuchal translucency, especially in monochorionic gestation, may indicate twin-to-twin transfusion syndrome. Establishing chorionicity and the number of fetuses is also easier in the first trimester.

Twin pregnancy in single amniotic sac
"If you are very early on in a monochorionic gestation, it becomes difficult to see a dividing membrane," Abu-Rustum says. "Use the transvaginal route, and you can count the yolk sac."
Abnormalities Detected by First-Trimester Ultrasound
Ultrasound in the first trimester can offer significant clues to diagnosis and reveal various hidden markers. One example is the butterfly sign, which refers to the normal appearance of the choroid plexuses on axial imaging. The absence of the butterfly sign can suggest holoprosencephaly, the failure of the forebrain to divide into the left and right halves.
The ductus venosus is an important structure not just for screening for aneuploidy but also for detecting complex venous malformations. With a normal venous system, you can see the right atrium, inferior and superior hepatic veins and the ductus venosus.
"One of my astute sonographers was scanning this first-trimester fetus, and she kept getting this circular vascular ring," Abu-Rustum recollects. "This was a portosystemic shunt that was picked up in the first trimester."
The Limitations of First-Trimester Ultrasound
Although ultrasound has several benefits in the first trimester, this tool also has a few limitations. Scanning a fetus in early pregnancy requires advanced training and high-end machines to be able to detect abnormalities.
"We are limited by maternal BMI, although under the pannus and the transvaginal route give us another option," Abu-Rustum says.
Additionally, early scanning is limited by the development stage of the fetus, can be time-consuming, and may cause undue anxiety for the parents. There are greater challenges with low-risk patients, so sonographers must be careful when they interpret ultrasounds. It's also critical to double-check and bring patients back if there are concerns about the fetus's development.
"I start with this example at 9 weeks, 5 days, where it looked like there's an omphalocele. Of course, we know that there is a normal example at this point in gestation. Bringing the patient back three weeks later, sweeping down, we have an intact abdominal wall with a normal cord insertion here, and this is physiologic gut herniation," Abu-Rustum recalls.
Performing an ultrasound scan at 12 to 14 weeks, adhering to guidelines and being mindful of safety recommendations is critical for ensuring the baby is developing properly.
Abu-Rustum says, "There are so many hidden markers that we can look for, and the future has unlimited potential."
Watch Prof. Abu-Rustum's full session HERE.