Evidence-based placenta accreta spectrum ultrasound findings offer a current and accurate approach to diagnosing this potentially dangerous condition during pregnancy. Becoming familiar with relevant ultrasound features helps sonographers and OB/GYNs identify possible concerns and address them before delivery.
Identifying Warning Signs in the First Trimester
Although placenta accreta spectrum does not yet exist in the first trimester of pregnancy, a skilled clinician may be able to identify precursor features such as a cesarean scar pregnancy. For patients with a previous cesarean section, a gestational sac in the lower uterine segment is a red flag for cesarean scar pregnancy. It can also lead to future placenta accreta if left untreated, according to a landmark paper published in Obstetrics and Gynecology.
Research published in BJOG defines a cesarean scar pregnancy as a gestational sac located low in the uterus, close to the internal os and anterior implantation, with the trophoblast invading into the myometrium. According to The ESHRE working group on Ectopic Pregnancy, the uterine artery can act as a landmark to define the level of the internal os using color Doppler.
Beyond identifying cesarean scar pregnancy, bulging of the gestation into the bladder may be a point of concern. (A patient's bladder must be moderately full during the exam for this to be observable.) Furthermore, the loss of the clear zone in the first trimester has high sensitivity and specificity for placenta accreta spectrum. The clear zone is defined as a regular hypoechoic plane in the myometrium beneath the placental bed. Instead of its normal appearance, it appears as irregular or is absent altogether.
The sooner cesarean scar pregnancy is diagnosed, the sooner patients can discuss treatment approaches, such as ultrasound-guided curettage, hysteroscopic resection, and laparoscopic-guided resection and repair. Surgical treatment of this form of ectopic pregnancy has a better safety profile at earlier gestations, before the late first or early second trimester.
Placenta Accreta Spectrum Ultrasound Findings in the Second and Third Trimesters
If a cesarean scar pregnancy is not identified early on — or if a patient and providers decide to knowingly proceed with a cesarean scar pregnancy — placenta accreta spectrum ultrasound findings may show up at the fetal anatomy (morphology) ultrasound between 18-20 weeks gestational age.
Since routine evaluation for placenta accreta spectrum is not standardized, sonographers and sonologists must look for certain markers that raise suspicion for the condition before a direct assessment. The combination of a previous cesarean delivery and persistent placenta previa at the time of delivery is the strongest marker for placenta accreta spectrum.
Providers should systematically search for several other key findings as they assess risk factors.
Placental Lacunae
These lakes of vascularity within placental parenchyma have a heterogenous appearance. It is possible to classify placental lacunae by the appearance of irregular, hypoechoic spaces with vascular flow within the placenta.
A large size or number of lacunae — especially more than three — may indicate a higher risk for placenta accreta spectrum. Conversely, the absence of lacunae in pregnancies with placenta previa and previous cesarean delivery has a high negative predictive value and often signifies no placenta accreta spectrum.
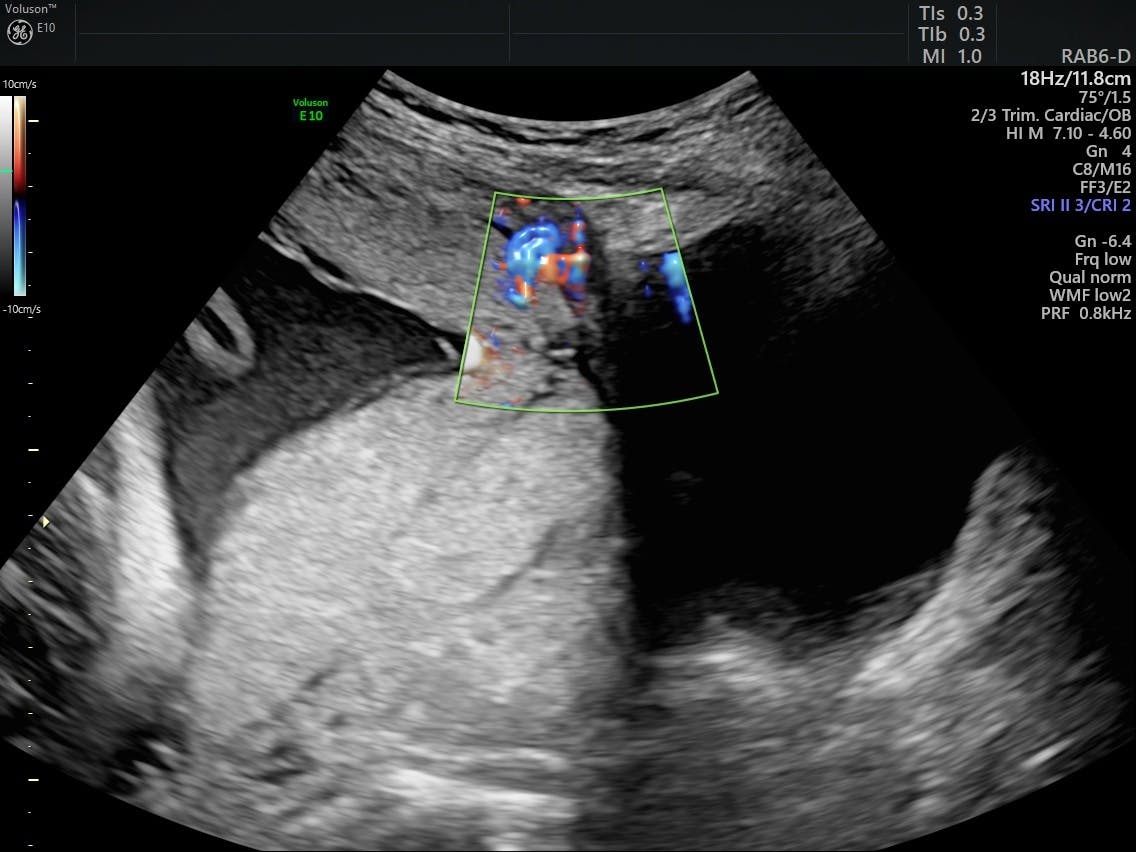
Abnormal Uteroplacental Interface
This feature is an extension of the loss of the clear zone. In addition to the loss of the retroplacental hypoechoic zone between the myometrium and the placenta, OB/GYNs should look for marked myometrial thickness of less than 1 mm and increased vascularity on color Doppler.
Myometrial thinning is a more controversial finding: Its presence may be more likely in patients with a history of cesarean delivery and in patients with normal pregnancies at a later gestational age, and it can be iatrogenically yielded with excessive transducer pressure.
Abnormal Uterovesical Interface
The uterovesical interface, or the space between the uterus and the bladder, may exhibit one or more key features, such as:
- Bridging vessels. An interruption in the interface between the uterus and the bladder may be clear on grayscale imaging. Color Doppler also clearly highlights bridging vessels.
- Interruption of the bladder wall. This is generally considered a specific feature of placenta accreta spectrum, especially if placental tissue is visible extruding through the interruption of the hyperechoic bladder wall. This may be associated with bridging vessels, or it may be unrelated.
- Increased vascularity between the uterus and bladder. Unlike bridging vessels, this feature does not quite interrupt the interface between the uterus and bladder. Rather, it is an area of significant vascular flow within the interface. It is possible to have both bridging vessels and increased vascularity in the uterovesical space. Importantly, a hypervascular area could be present in the absence of placenta accreta spectrum and in the setting of placenta previa; providers should proceed with caution if this is the sole feature of placenta accreta spectrum.
- Placental bulge. Placental bulge is visible as a deviation of the uterine serosa away from the expected planes. The typical contour of the uterus is changed secondary to the placental bulge. In some cases, this bulge can be so severe that placental tissue is visible extruding beyond the uterine serosa, which would then also be classified as interruption of the bladder wall.
Separation Sign
The most recently identified feature of placenta accreta, described in an Ultrasound in Obstetrics and Gynecology paper in 2022, is called the separation sign. An ultrasound operator can attempt to detect different elasticities between the myometrium and placenta by looking for different rates of rebound when the uteroplacental interface is bounced with the probe.
Applying similar nomenclature to the sliding sign used in endometriosis ultrasound, a positive test indicates a degree of movement between the myometrium and the placenta. In performing the separation sign test, the clear zone, which is often lost in placenta accreta spectrum, is exaggerated and more easily visualized.
Ultrasound Is Key to Safely Detecting Placenta Accreta
Besides being a primary mode of detecting the numerous features indicating placenta accreta spectrum, ultrasound is a cost-effective, safe and readily available tool for pregnancy assessment. Providers who have not yet considered this option can adopt placenta accreta spectrum ultrasound protocols with help from practical guides and professional organizations. Ultrasound may also help patients avoid unnecessary and expensive MRI assessments, which are still commonplace in many practices.
Placenta accreta spectrum should no longer be a surprise at the time of delivery. Placenta accreta ultrasound findings allow for an appropriately planned delivery in the right setting and with the right team.