Uterine myomas or leiomyomas, commonly known as fibroids, occur in 1 in 5 women in their childbearing years and can sometimes affect fertility. Thankfully, this prevalent diagnosis is now matched by a growing arsenal of fibroids treatment options designed to manage symptoms without eliminating future fertility.
Among these options is fibroid ablation therapy, which offers numerous advantages for patients, such as a minimally invasive approach, faster outpatient recovery and fertility preservation.
Risk Factors for Fibroids
Fibroids are most common in women between the ages of 30 and 40, but they can appear at any age, according to the American College of Obstetricians and Gynecologists. Risk factors include obesity, family history, nulliparity and race. Notably, these growths are found in up to 80 percent of Black women, according to the American Society for Reproductive Medicine (ASRM). Black patients with fibroids tend to experience more severe symptoms and experience larger and more numerous growths.
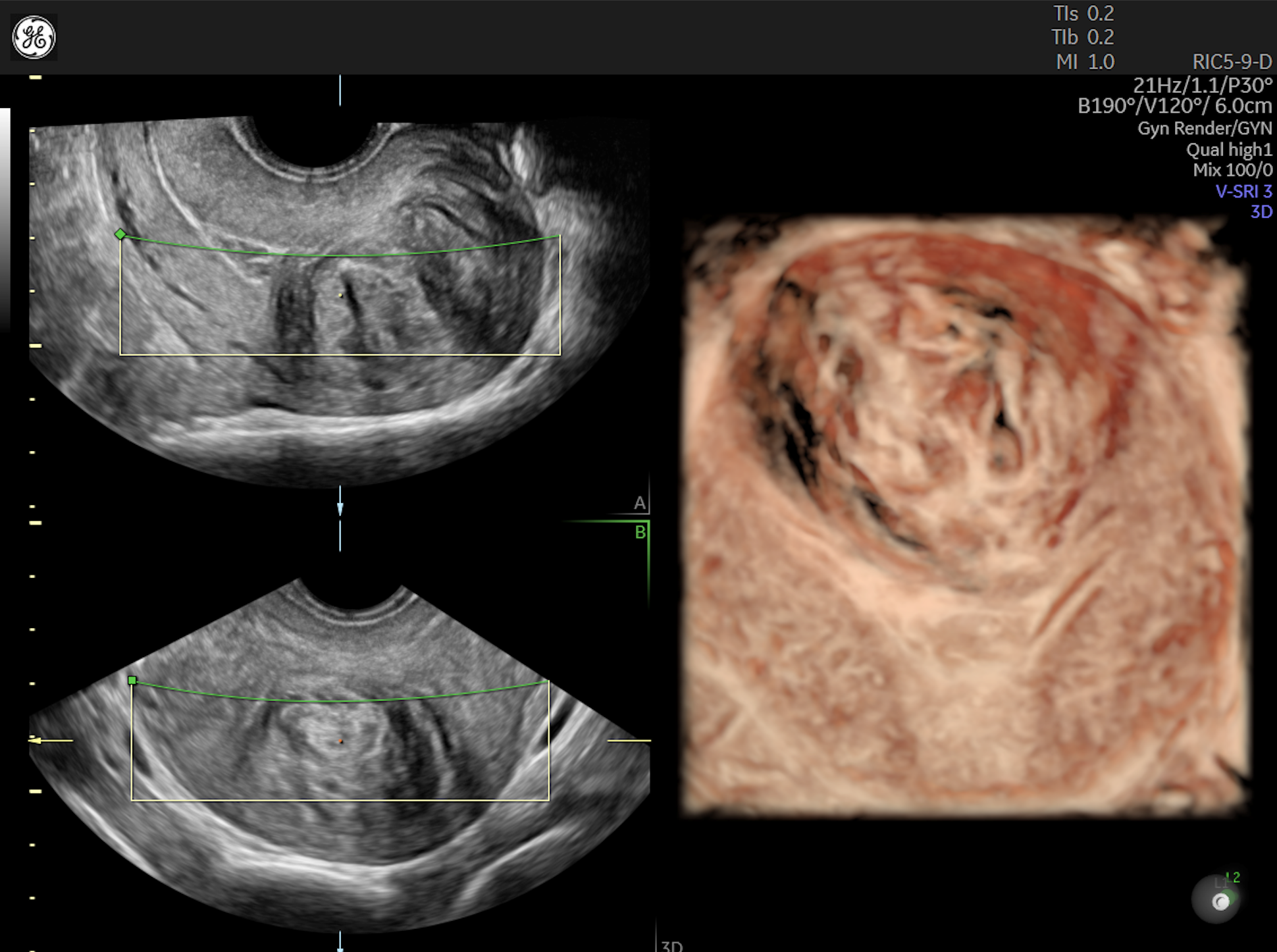
Fibroid seen on ultrasound rendered with HDlive™ Studio
The chief symptom of fibroids is abnormal vaginal bleeding, which occurs in roughly 30 percent of women with these growths. Other symptoms include pelvic pain and pressure, dyspareunia, anemia, frequent urination, problems defecating and infertility.
ASRM reports that roughly 5 percent to 10 percent of women who are unable to conceive have fibroids. The first step to address these growths is confirming a diagnosis.
How Does Ultrasound Aid in Diagnosis?
Fibroids are often detected during a routine pelvic examination if the uterus feels enlarged, irregular and firm. Other conditions must initially be ruled out, as a differential diagnosis might include ovarian neoplasm, adenomyosis or pregnancy.
Ultrasonography is generally the first-line imaging method for pelvic masses. Transvaginal ultrasonography paired with uterine injection of saline may provide additional information about growths in the endometrial cavity. Furthermore, ultrasonography may prove more helpful than hysteroscopy for measuring and mapping intramural fibroids, which lie in the muscular uterine wall, and submucosal fibroids, which project into the uterus, reports research published in Obstetrics and Gynaecology Cases Review. Categorizing fibroids by noting the size, location and number of growths can help to inform clinical decision-making about the right method of treatment.
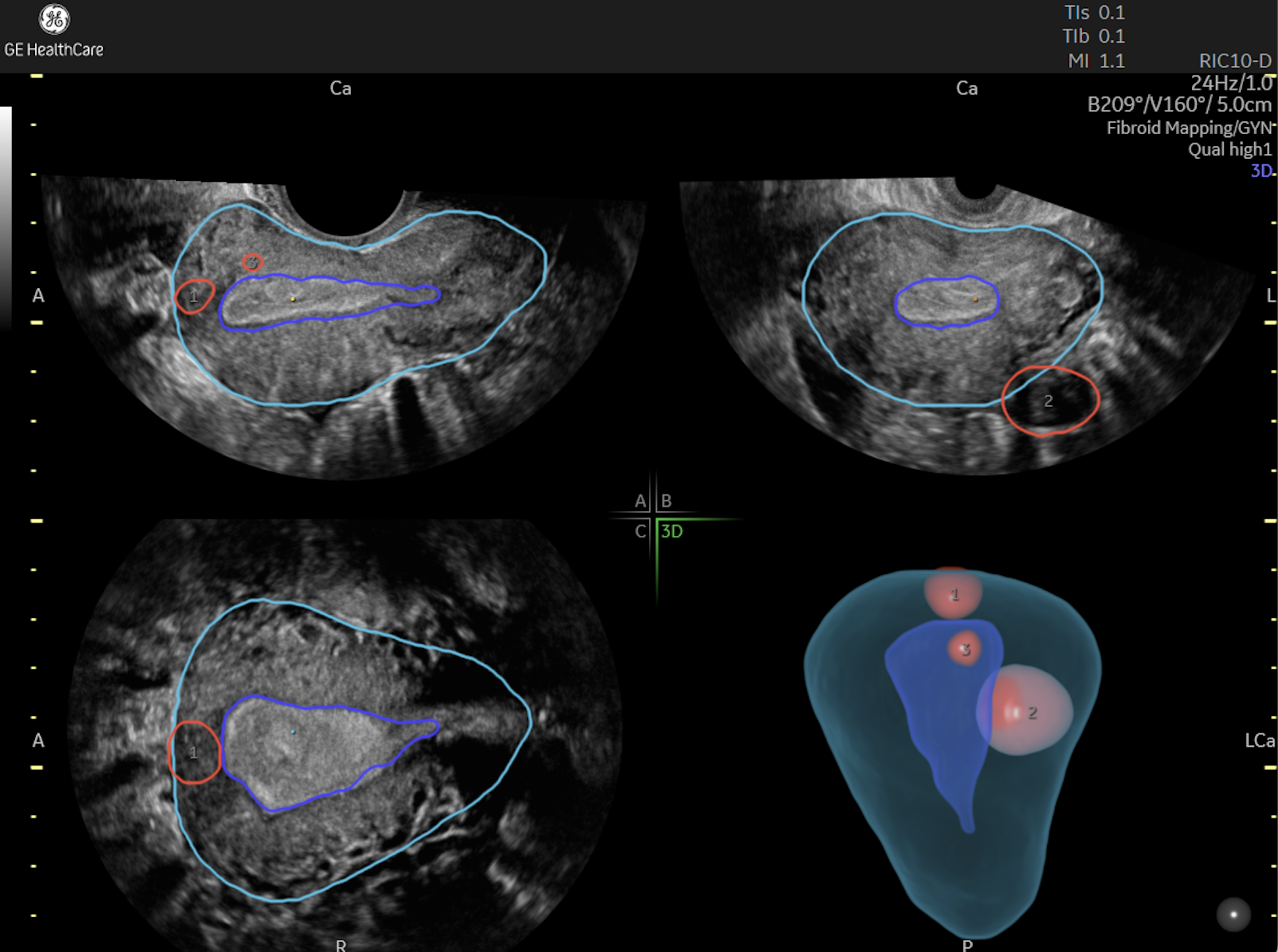
RIC-10 probe used to see Fibroid rendered with Voluson™ Fibroid Mapping tool
Approaching Fibroid Treatment
As long as cancer is not a concern, the decision to treat symptomatic fibroids is largely a quality-of-life issue shaped by your patient's fertility goals. Medical therapy aims to ease symptoms; minimally invasive procedures endeavor to relieve symptoms by shrinking or destroying fibroids while sparing healthy tissue. Historically, treatment options for symptomatic fibroids in patients who wished to become pregnant centered on medical management, myomectomy or uterine artery embolization (UAE).
With medical management, ACOG generally recommends starting with some form of hormonal treatment. This may take the form of an oral contraceptive, progestin-releasing IUD or gonadotropin-releasing hormone agonists. If these approaches fail to give a patient significant relief, or if patients are trying to conceive, surgical treatment may be the next step.
Myomectomy is the most common fertility-preserving surgical treatment of fibroids. The procedure can be performed via several different routes, although most are performed by laparotomy, reports research published in Obstetrics and Gynaecology Cases Review.
Hysteroscopic myomectomy may be employed to remove submucosal fibroids. However, its failure rate ranges as high as 35 percent. Success is mainly determined by the size of the tumor and its extension into the endometrial cavity. Additional treatments may be needed to manage bleeding. In one study, 69 percent of participants experienced relief from bleeding after one surgery, and 88 percent found relief after three surgeries.
Yet, surgical removal of several fibroids may affect patients' ability to conceive, cautions a 2018 study published in the Journal of Minimally Invasive Gynecology. Women who had six or more fibroids surgically removed with robotic, laparoscopic or abdominal myomectomy were significantly less likely to go on to conceive than women who had fewer growths removed — 22.9 percent vs. 70.8 percent, respectively.
Moving Toward a Minimally Invasive Alternative
A newer and often appealing option to preserve fertility in women with fibroids is ablation, which may be referred to in the literature as magnetic resonance-guided focused ultrasound surgery. As the name suggests, this method sends targeted, high-intensity waves of ultrasound energy through the abdominal wall to destroy the fibroid mass.
Optimal results with fibroid ablation therapy begin with confirming the diagnosis of fibroids, as the growths may mimic other conditions, recommends a practice guideline in European Radiology. Careful patient selection is a critical next step. The most treatable fibroids tend to be accessible and solitary, with a diameter of 10 centimeters or less and low signal intensity. Ultrasound may prove useful for illuminating the number, size, signal intensity and vascularization of the growths prior to treatment.
Patients for whom this treatment is not recommended include those who have a body weight above 115 kilograms (about 250 pounds), anemia, certain implanted devices or allergies to gadolinium-based contrast agents. Further, because of the potential for fibroids to recur before menopause, younger patients interested in this option may require counselling about the risk of needing additional treatments.
Patients with multiple fibroids and who have larger growths also are also more likely to need additional treatments compared with those with a single fibroid or small ones. For these patients, an open discussion of ultrasound findings may help set realistic expectations about fibroid ablation therapy.
Creating Lasting Symptomatic Relief
Depending on the patient, ablation may be performed on an outpatient basis or require a short hospital stay. Following treatment, fibroids tend to shrink over the ensuing weeks and months, gradually lessening symptoms.
Patients in a 2013 clinical trial published via the National Institutes of Health reported a significant improvement in symptoms as early as three months after treatment along with a better quality of life. The procedure also may provide lasting symptomatic relief: 88 percent of treated patients reported significant relief from symptoms even a year after treatment, notes research from the Journal of Vascular and Interventional Radiology.
Serious complications occur in just 1.1 percent of patients, according to a fairly sizable cohort study in the European Journal of Obstetrics & Gynecology and Reproductive Biology. The most common complication, mild to moderate pain, was reported by 6.4 percent of patients in the study group.
Although fibroid ablation may be performed on an outpatient basis, patients who are hospitalized after treatment tend to leave the hospital earlier and return to full activity more quickly than those undergoing UAE or myomectomy.
Addressing Pregnancy After Fibroids Treatment
For patients who wish to start or add to their families, fibroid ablation therapy appears to increase the possibility of conception when compared to uterine artery embolization, reports a multicenter retrospective study in Fertility and Sterility. Women in the study group conceived eight months after treatment, on average, and a total of 54 pregnancies were reported among 51 women. Of those, 41 percent resulted in live births, while 28 percent were miscarried and 11 percent were electively terminated.
Following treatment, transvaginal ultrasound is an effective method to check for the development of new fibroids. This is particularly important among younger patients, who are more prone to recurrence.
A thoughtful fibroid management approach considers a patient's fertility goals and quality of life as part of a shared decision-making process. The advent of newer fibroid treatments for this common condition can provide both clinicians and patients with even more choices.