Artificial intelligence (AI) and predictive or monitoring technology are rapidly gaining traction in healthcare across all specialties. Advanced urogynecology technology, from robotic surgery to wearable devices for incontinence, is poised to transform how OB/GYNs deliver care.
AI in Healthcare: Looking Toward the Future
Artificial Intelligence (AI) has become part of our everyday lives—reducing tasks and simplifying our daily routines. In a healthcare context, AI generally refers to algorithms that use vast troves of patient data to help predict outcomes, aid in making a diagnosis and offer clinical decision support.
This technology is not at a point where machines can think and rationalize independently. But they can analyze large sets of data quickly and can help clinicians detect and diagnose earlier, help choose treatment paths tailored to patients, or help predict the risk for negative outcomes. AI technology does not replace the work of human clinicians but complements it.
As an industry, AI in healthcare is poised to grow to more than $120 billion in market size by 2028, according to Grand View Research, Inc.
Advances in Technology for Urogynecology
Using large amounts of data and emerging technologies can benefit patient care in a few key ways:
- More precisely staging disease
- Integrating data across multiple systems and users
- Improving efficiency in care delivery
- Remotely monitoring patients
Many systems are still in early development and in the clinical trial phase. Here is a look at what is currently available and what is coming.
Ultrasound
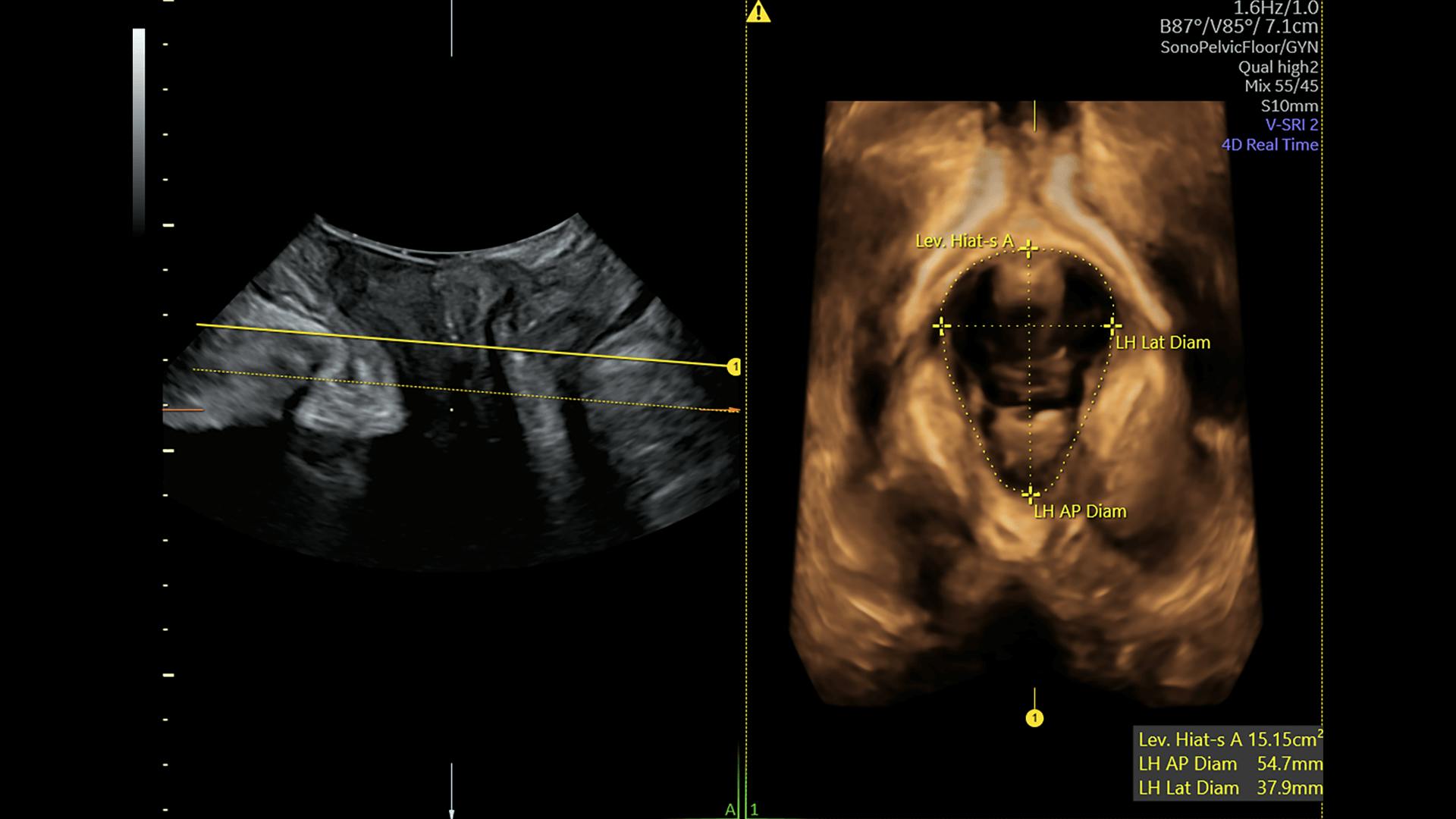
AI is also beginning to play an important role in women's health ultrasound, helping to improve the delivery of care and efficiency of ultrasound exams. Ultrasound systems, like the Voluson™ family of products, contain AI tools to help clinicians be more efficient, allowing them to reduce repetitive tasks and focus on patients and practice needs.
One example of an AI ultrasound tool, dedicated to urogynecology clinicians, is SonoPelvicFloor. Analysis of the pelvic floor anatomy can be complicated. Using a guided workflow and AI, Voluson™ SonoPelvicFloor removes the complexity of assessing pelvic floor anatomy. It simplifies the 3D exam process for clinicians by automating plane alignment, measurements, and workflow guidance to eliminate uncertainty while improving efficiency. SonoPelvicFloor can reduce exam time by 87% over manual examinations, allowing clinicians to spend more time with patients.
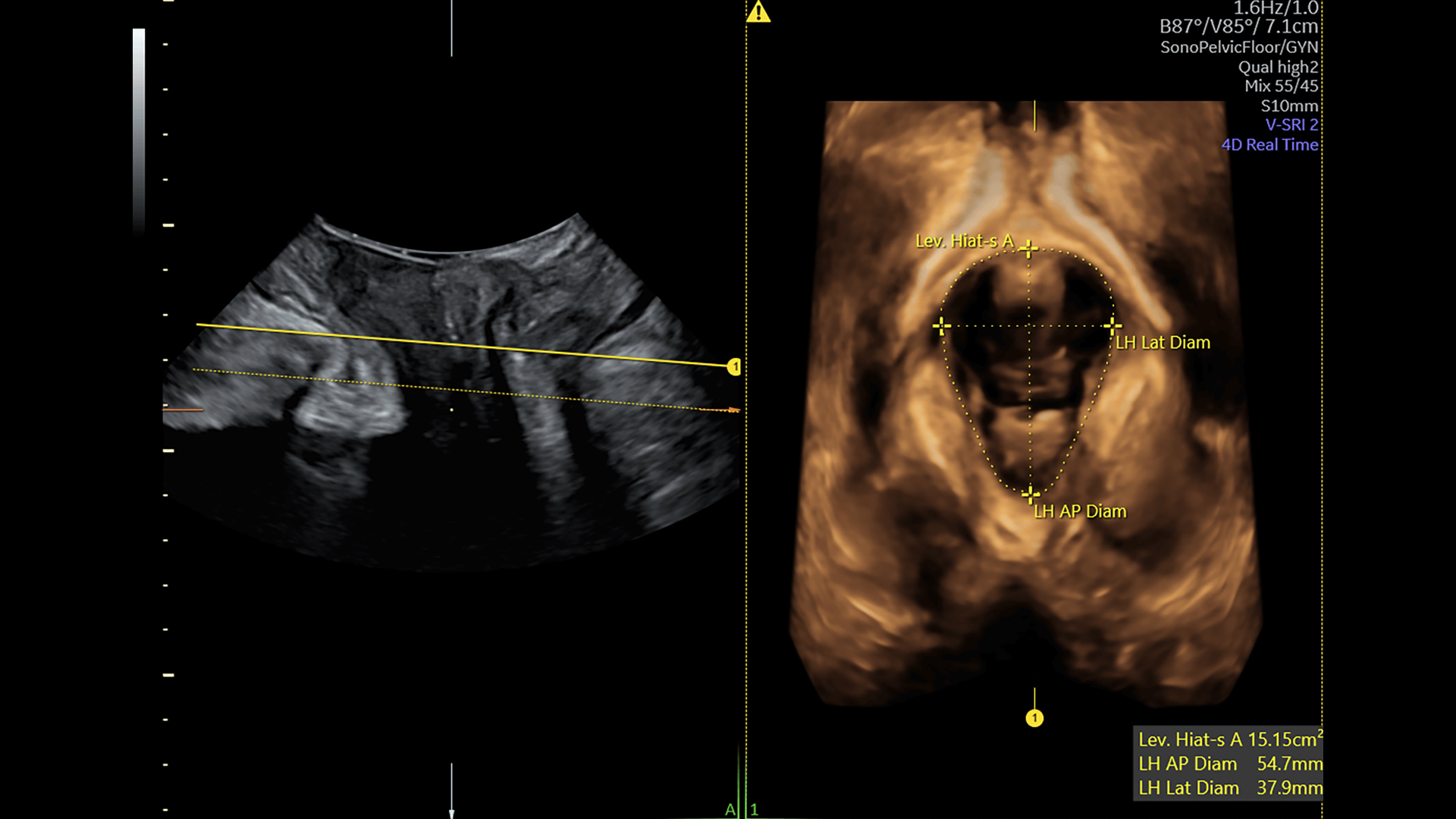
Using a guided workflow and AI, SonoPelvicFloor removes the complexity of assessing pelvic floor anatomy and can reduce exam time by 87% over manual examinations.
Surgery
Robotic surgery is common in sacrocolpopexy and other gynecologic procedures. A comprehensive review published in the Journal of Clinical Medicine even evaluated the use of augmented reality with robotic surgery for urological and related procedures, particularly kidney removal.
Algorithms in development can also help predict outcomes after prolapse surgery. These are still in development and need more research validation, but the goal would be to develop algorithms that can recommend personalized solutions for each patient before or after surgery.
Diagnosing Urinary Conditions
Many women experience urinary incontinence, but the condition remains undertreated, especially in lower-income countries. That problem could be alleviated by using algorithms to screen urine and detect urinary tract infections.
Research published in the Open Journal of Obstetrics and Gynecology proposes a similar algorithm for urinary incontinence. An ideal system would detect incontinence and would include sensors to deliver treatment, such as electrical stimulation, and monitor the patient over time.
Researchers in the Cedars-Sinai Medical Center looked at algorithms to classify patients into phenotypic-specific groups for management of lower urinary tract symptoms, such as urinary frequency, painful urination and bladder discomfort. The proposed algorithm had a diagnostic accuracy of nearly 90 percent, which could allow physicians to make a diagnosis without the need for additional testing and evaluations.
Wearables and Personal Devices
A growing body of wearable or personal devices for urinary incontinence and pelvic floor muscle strengthening can improve patients' ability to manage their pelvic health. Once patients get an accurate diagnosis, they need manageable treatment options. Wearables and trackers can make it easy for patients to manage their conditions at home.
INNOVO is one option that uses electrical stimulation to target weakened pelvic floor muscles in an effort to treat stress urinary incontinence. This device is now available over the counter.
The DFree wearable device uses ultrasound technology to detect bladder changes, predict when patients may need to urinate and send alerts to their phones. Users can also track their toilet patterns, which can lead to more accurate histories during office visits.
Pelvic floor muscle trainers, such as Elvie and Squeezy, encourage patients to perform Kegel exercises. The Elvie offers biofeedback and gamification elements to encourage regular use.
The Future of Urogynecology Technology
Many advanced urogynecology technologies are still in development, but this field of study is moving forward quickly. The use of algorithms and predictive analytics can help improve clinical decision support, ensuring accurate diagnoses and predicting outcomes to allow for early interventions.
Wearables and other devices provide support to patients outside of the office to help them know how to manage their condition and track symptoms. This additional information has the potential to improve quality of life and patient satisfaction.