For decades, ultrasound has proven to be a reliable and minimally invasive imaging modality that can supply doctors with a wealth of knowledge about the inner workings of the human body. As this technology improves, the increased use of ultrasound in gynecology is allowing clinicians to make quicker diagnoses and more confident decisions in both routine and complex exams and pathologies.
Other modalities traditionally used for diagnostic imaging, such as magnetic resonance imaging (MRI), computed tomography (CT) and hysterosalpingogram, all have drawbacks related to cost, wait times, radiation or complexity of interpretation. Diagnostic ultrasound does not expose patients or physicians to ionizing radiation and is at least as accurate as MRI for identifying Müllerian duct anomalies and other uterine malformations, according to research published in the Journal of Ultrasound in Medicine.
Benefits of Ultrasound for Diagnostic Imaging
Ultrasound is safe, nonionizing, effective, affordable, easy to learn and simple to interpret. It provides immediate results, allows for live assessment of organs and pain points, and can easily be shared with colleagues. Having this invaluable imaging modality right in the office can benefit gynecology practitioners and patients in myriad ways. Below are some of the most significant benefits of ultrasound in gynecology.
Inexpensive imaging: CT, MRI and hysterosalpingogram are simply more expensive than ultrasound, and the expense of diagnostic exams is a real barrier for some patients. Ultrasound enables clinicians to provide effective imaging for better patient care with lower overhead costs and fewer copays.
Full visualization of gynecological anatomy: 3D ultrasound provides a view of the coronal plane, which allows for more realistic and complete imaging of internal pelvic organs. Pathology within or around the pelvis is easier to see and understand with 3D ultrasound, especially in relation to other organs and tissue layers.
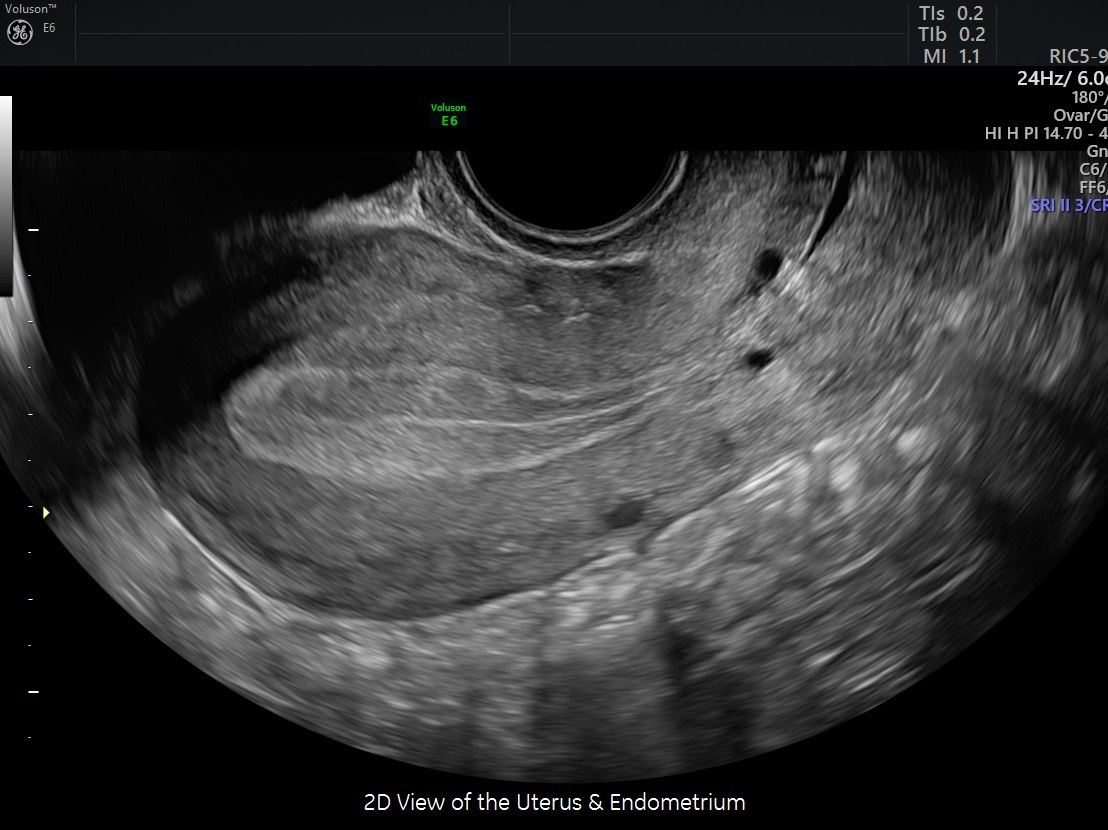
A 2D diagnostic ultrasound view of the uterus
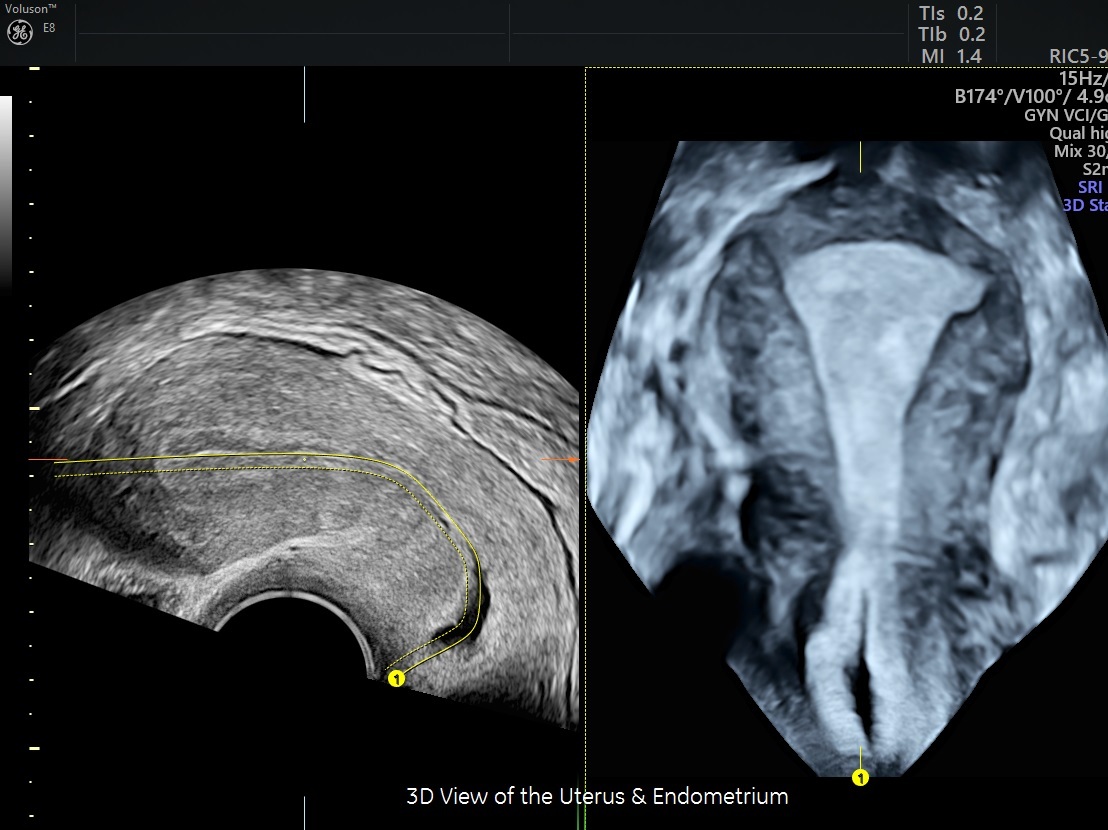
Full diagnostic ultrasound view of the uterus
Dynamic and interactive exams: Real-time examination yields valuable information that often cannot be gained through the assessment of static images. The application of pressure and use of a transvaginal probe makes it possible to define specific locations of pain, determine elasticity of pelvic contents, evaluate deep pelvic masses and their possible adherences, witness sliding of tissue layers, and evaluate the bowel in relation to pelvic organs.
Reduced travel and wait times: Ultrasound is accessible and portable enough for clinicians to have in-house. This eliminates the need for patients to travel to other facilities or make additional appointments, and it can improve the time to diagnosis for more complex and painful gynecological disorders.
No radiation: For practices that often work with patients of reproductive age, a reliable, nonionizing imaging option is integral to a positive patient experience. Diagnostic imaging using ultrasound allows for a thorough assessment of the pelvic organs without concern of future negative effects due to radiation.
Immediate results: Ultrasound is live and provides a unique opportunity to view pathology in real time. Interpretation and evaluation can be conducted immediately after the exam, and a treatment plan can be discussed with the patient during the same appointment, saving time and money for both parties.
Seamless sharing of images: Many ultrasound systems include image sharing tools, such as Tricefy, that connect physicians with their colleagues and patients for collaboration, second opinions, remote viewing and archiving.
A Sound Investment for Your Clinical Practice
The convenience, cost-effectiveness and safety of ultrasound make it the best tool for gynecological evaluation. It enables clinicians to diagnose patients with greater confidence and build trust by providing immediate answers to patients' most pressing questions. Diagnostic ultrasound also boosts efficiency by minimizing wait times and providing a platform for physicians to collaborate with colleagues and patients simply and securely. By using ultrasound as a first-line diagnostic tool, clinicians can improve patient outcomes and drive growth for their practices.