
Why Ultrasound Is Crucial in Diagnosing Maternal Birth Injury
Checking for Pelvic Floor Injuries

At the patient’s six-week postpartum appointment, most OBGYNs are focused on healing and recovery, not checking for pelvic floor injuries.

Up to half of all women suffer some form of pelvic floor muscle damage from childbirth.1
Trauma can lead to embarrassing bowel and bladder control problems—and without a timely diagnosis, many women are suffering for years without treatment.
You’re trained to inspect her incisions. Make sure her ovaries, cervix and uterus are returning to their pre-pregnancy size. At the patient’s six-week postpartum appointment, most OBGYNs are focused on healing and recovery, not checking for pelvic floor injuries.
Dr. Hans Peter Dietz, University of Sydney Professor of Obstetrics and Gynecology, believes many childbirth-related injuries are overlooked because there’s a big problem with the standard postpartum checkup.
“The standard assessment is just a basic pelvic exam and it’s woefully inadequate,” Diez stressed. “It only evaluates surface anatomy. Commonly, we have no idea what’s happening beneath the surface.”
OBGYNs expect many women will experience some tearing during delivery, but research now shows that up to half of all women giving birth to their first child vaginally will suffer some degree of permanent damage to their levator ani or anal sphincter muscles.1 The weakening of the levator ani or pelvic floor muscle can increase the risk of pelvic organ prolapse. In fact, an estimated 10 to 20 percent of women will undergo surgery for this condition at least once in their lifetime.2,3

It’s also clear that anal sphincter trauma is much more common than generally assumed and frequently missed in the delivery room.
A study of 320 women found 28 percent of patients who delivered vaginally had anal sphincter injuries and 87 percent of them were not diagnosed in the delivery suite.4,5 With devastating effects like fecal and urinary incontinence and painful intercourse, childbirth-related injuries can severely undermine a woman’s quality of life.
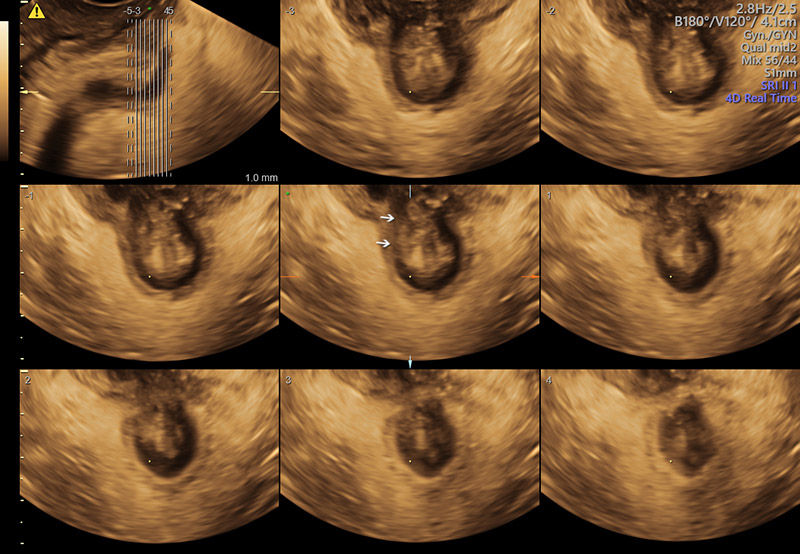
3D of pelvic floor demonstrating a tear in the external anal sphincter.
Incontinence is a huge source of shame and anxiety. Countless women experience the daily horror of losing bladder and bowel control, and with that uncertainty comes constant worry: ‘Will I make it to the bathroom on time?’ ‘Will anyone notice the wet spot on my pants?’ The embarrassment can shatter self-confidence, ruin intimacy and lead to isolation. In some cultures, women carry the added burden of being labeled ‘unclean’ and are restricted from certain religious and social activities.
Significant developments in imaging over the past several years have led to a better understanding of the nature of these injuries. GE’s Voluson™ technology has enabled physicians to detect postpartum trauma more accurately and with greater ease—which has provided the opportunity for earlier interventions and more treatment options.
“Much of what we deal with in our field is invisible on the outside. We need to get the diagnosis right—and you do that with imaging. That’s the key to secondary prevention and early treatment of pelvic floor problems,” Dietz said.
Voluson’s Tomographic Ultrasound Imaging, or TUI, allows users to visualize parts of the anatomy in greater detail by displaying simultaneous slices of 3D multiplanar images. You can also evaluate volumes faster than ever before because the block of imaging data is renewed several times a second.
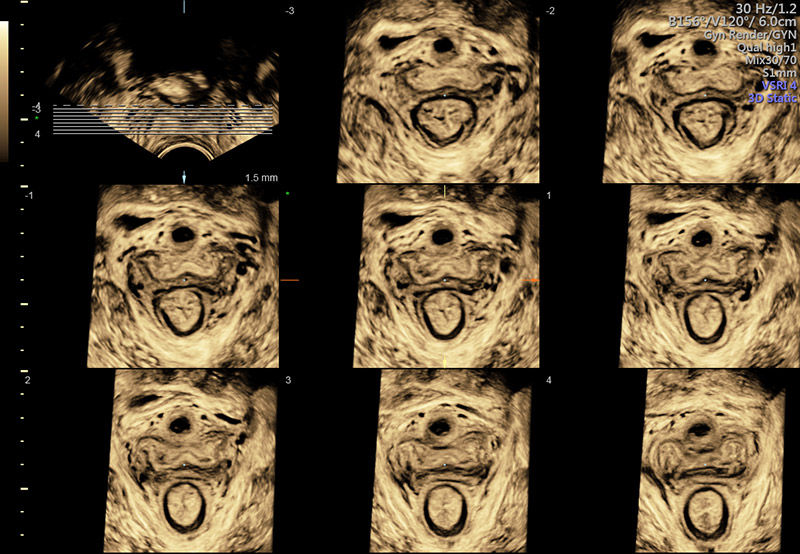
3D of normal pelvic floor in TUI display ( tomographic ultrasound imaging).
“3D and 4D imaging have had a major impact on urogynecology because the scans provide access to the axial plane and make it easier to understand spatial relationships with sectional planes.”
Dietz adds,“The Voluson E10 is clearly superior to any other machine I know for sphincter imaging.”
Not only does ultrasound play an integral role in diagnosis, it’s critical in surgical planning and provides valuable insights in determining treatment approaches. This is particularly true in women with sling and mesh complications, a topic that has attracted a lot of attention recently. Ultrasound advancements are also spurring new treatments and surgical innovation.
Despite the substantial benefits, Dietz has dedicated much of his career trying to convince physicians to utilize ultrasound more in diagnosing pelvic floor dysfunction.
“We are making headway, but many of our colleagues have done the same thing for 20 or 30 or 40 years. It’s hard to change tack and learn something completely new when you’ve considered yourself an expert in a field for decades—even if the benefits are obvious.”
For Dietz, it’s very simple: “Why would you remain blind, if you could see?”
-
Learn from Dr. Dietz how to image for pelvic floor dysfunction in this educational video.
-
A step-by-step guide from Dr. Dietz on how to use ultrasound to image for pelvic floor dysfunction.
Shek K, Dietz H. Intrapartum Risk Factors of Levator Trauma. BJOG. 2010; 117:1485-1492.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of Surgically Managed Pelvic Organ Prolapse and Urinary Incontinence. Obstet Gynecolo. 1997;89:501-506.
Smith F, Holman D, Moorin R, Tsokos N. Lifetime Risk of Undergong Surgery for Pelvic Organ Prolapse. Obstet Gynecolo. 2010;116:1096-1100.
Andrews A, Sultan A, Thakar R, Jones P. Occult Anal Sphincter Injuries-Myth or Reality? BJOG. 2006;113:195-200.
Guzman Rojas R, Shek K, Langer S, Dietz H. Prevalance of Anal Sphincter Injury in Primiparous Women. Ultrasound Obstet Gynecol. 2013;42:461-466.


