As fertility patients transition from noninvasive treatments, such as timed intercourse to assisted reproductive technology, the question lingers: "If I need it, does insurance cover IVF?"
The answer to that question depends on a variety of factors, including the state where the patient is employed, their employer, their insurance company and the specific plan they have with them.
Infertility burdens patients not only emotionally and physically, but also financially. It's important that reproductive endocrinologists and other staff recognize this and do what they can to demystify insurance.
State Law Infertility Mandates
According to RESOLVE: The National Infertility Association, 16 states have infertility insurance mandates and four have fertility preservation laws — but there are exceptions. Patients should ask their employers:
- Whether the plan is fully insured or self-insured. Fully insured plans must follow the state law unless the employer falls under one of the exceptions below. Self-insured plans, however, are exempt from state law and instead follow federal law. Currently, no federal law mandates infertility coverage.
- The total number of employees. In many cases, companies with fewer than 25 — or sometimes 50 — employees do not have to offer coverage.
- The state in which the policy was written. If the policy was not written in a state that mandates infertility coverage, the employer is not required to offer it.
- Whether the organization is considered a religious institution. Often, religious organizations are not required to offer any or certain types of coverage.
Saline-infused Sonohysterogram of normal uterus.
Saline-infused Sonohysterogram of normal uterus
Further, there are two types of mandates:
- Mandate to cover: The law requires that health insurance companies provide coverage of infertility treatment in every policy.
- Mandate to offer: The law requires that health insurance companies make a policy that covers infertility treatment available for purchase, but employers are not required to do so.
Two states — California and Texas — have only a mandate to offer, but each state has its own exceptions to the overall law. However, it's also important to note that employers can elect to offer insurance coverage not mandated by the state.
Understanding Individual Coverage
To truly answer, "Does insurance cover IVF?" reproductive endocrinologists should direct patients to their current service benefit plan brochure. If the patient has not yet purchased health insurance, most companies readily provide these documents online.
If possible, a member of the fertility clinic's financial staff should go through patients' benefits with them. Although the brochure looks intimidating, they should draw their attention to three sections (exact names may vary):
- Family planning (likely a subsection under "Medical services and supplies provided by physicians and other healthcare professionals").
- Reproductive services (also likely a subsection under "Medical services and supplies provided by physicians and other healthcare professionals").
- Covered medications and supplies (likely a subsection under "Prescription drug benefits").
These sections combined should detail the patient's exact coverage. It's possible that the insurance covers infertility diagnostics, fertility drugs, inseminations, in vitro or a combination thereof, or nothing at all.
Approaching Employers for IVF Benefits
If the financial staff and patient discover that insurance doesn't cover IVF, all is not lost.
Oftentimes, employers do not realize their current plan doesn't meet the IVF needs of employees and would welcome a discussion about desired changes. To make this conversation successful, the financial staff should direct patients to the resources offered by RESOLVE.
Here is an overview of RESOLVE's workplace insurance coverage checklist:
- Determine the coverage plan type (i.e., fully insured, self-insured).
- Research whether or not the state has a mandate, and if so, what it entails.
- Identify the company's benefit plan decision-maker(s).
- Customize the Sample Letter for Employers Template.
- Draft an email that includes the customized letter, insurance coverage facts, evidence that fertility treatments are no longer experimental and the impact the new coverage would have on the employee's life.
Although RESOLVE doesn't mention it specifically, reproductive endocrinologists should consider writing a letter on behalf of the patient — with the patient's express permission, of course. This can include why infertility is not an elective disease, the treatment(s) the doctor thinks are medically necessary (now or in the future) and how the success rates compare with other treatments covered by the plan.
By working together and having a plan, healthcare professionals and their patients can navigate whether insurance plans cover IVF treatments.
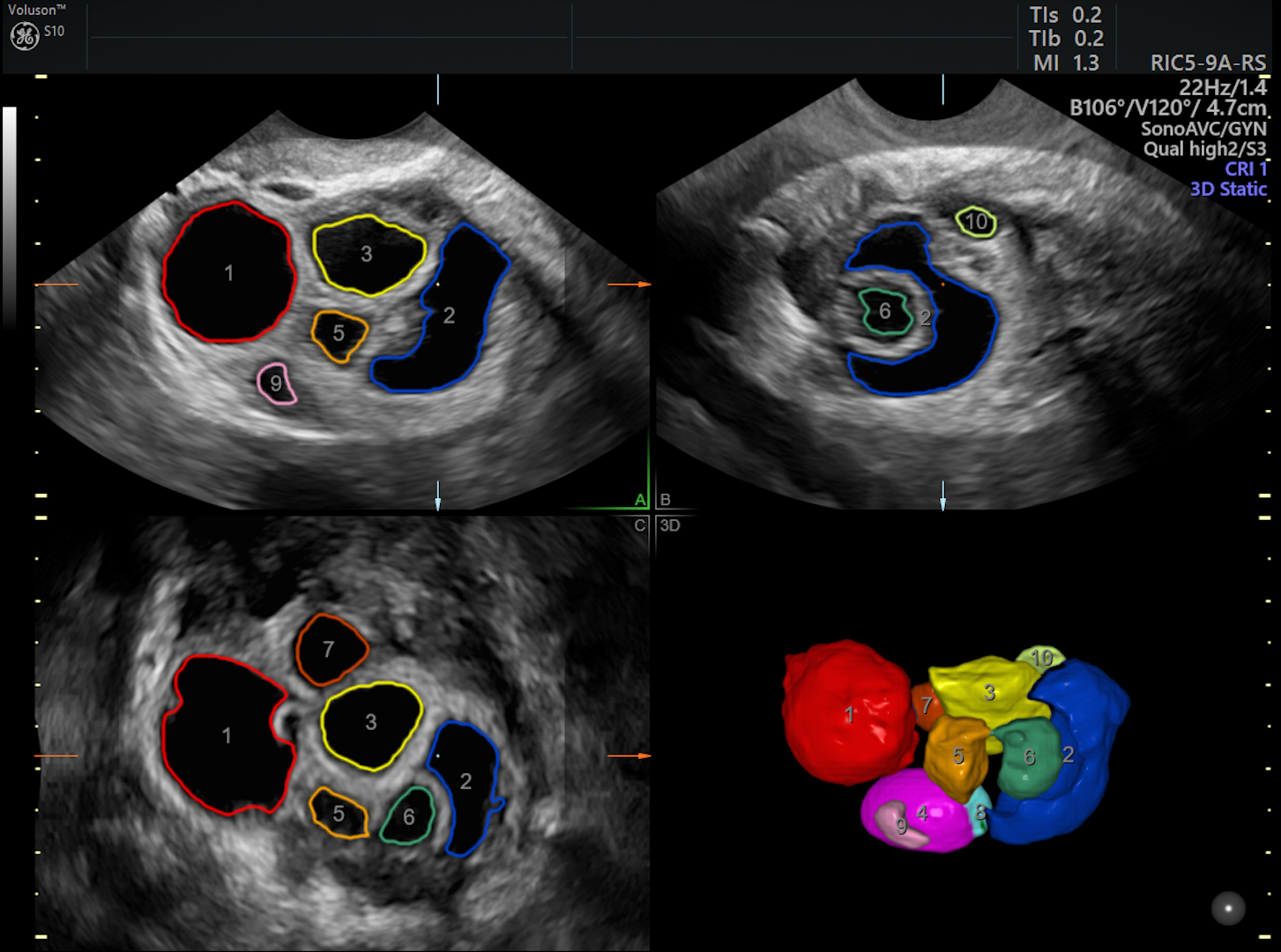
3D of ovarian follicles are counted and measured with SonoAVCfollicle
3D volume of stimulated ovary with automated measurement technology (SonoAVCfollicle)