In the emergency room (ER), women frequently present with complaints of acute pelvic pain. Unlike other conditions, which may have obvious causes, pelvic pain is often nondescript and can be from a gynecological, gastrointestinal, genitourinary or musculoskeletal source. This broad range of possibilities can make it difficult to arrive at an accurate pelvic pain diagnosis. It's essential to determine the cause of pelvic pain quickly, as some conditions that cause this symptom can be life-threatening.
A thorough assessment — including a physical examination, laboratory and imaging studies and questions about patient health history — is key for discovering the underlying cause of pelvic pain, especially if you suspect a gynecological problem.
First Steps to Diagnosing Pelvic Pain in the ER
When a patient presents to the ER with a chief complaint of pelvic pain, doctors should first seek out a thorough medical history, including the results of any prior laboratory or imaging studies. The patient's history will likely provide key clues to the cause of pelvic pain and can be used to guide diagnostic decisions going forward. Merck Manuals advises asking your patient about their gynecological history, including details about menstruation, gravity, parity and history of sexually transmitted diseases.
Next, a comprehensive review of symptoms helps gather more information needed to make a precise diagnosis. Specific symptoms accompanying pelvic pain, such as missed menses or breast tenderness, may suggest gynecological origins and can help rule out other body system involvement.
Physical Pelvic Pain Exams and Testing
An initial physical examination for suspected gynecological causes of pelvic pain should include bimanual examination, inspection of the external genitalia and speculum examination of internal reproductive structures. Following this, you may choose several tests to aid in the pelvic pain diagnostic process.
Laboratory tests such as urinalysis, complete blood count (CBC), hormone assay, beta-human chorionic gonadotropin (hCG) and sexually transmitted disease tests are all useful in narrowing down specific causes of pelvic pain, according to Medscape. Imaging studies frequently accompany these laboratory tests. Research published in the Journal of the American College of Radiology names transvaginal and transabdominal pelvic sonography as the procedure of choice for the evaluation of pelvic pain.
Ultrasound for Pelvic Pain Diagnosis
In acute care settings, ultrasonography is an accurate, less invasive and less expensive imaging option compared to other diagnostic tests for pelvic pain. Using ultrasound as a first line diagnostic test provides other benefits to the patient, such as greater comfort and convenience compared to other imaging tools like computerized tomography (CT) or magnetic resonance imaging.
Newer technologies, such as 3D ultrasound, may allow you to better visualize conditions such as pelvic inflammation, ruptured cysts or ectopic pregnancy.
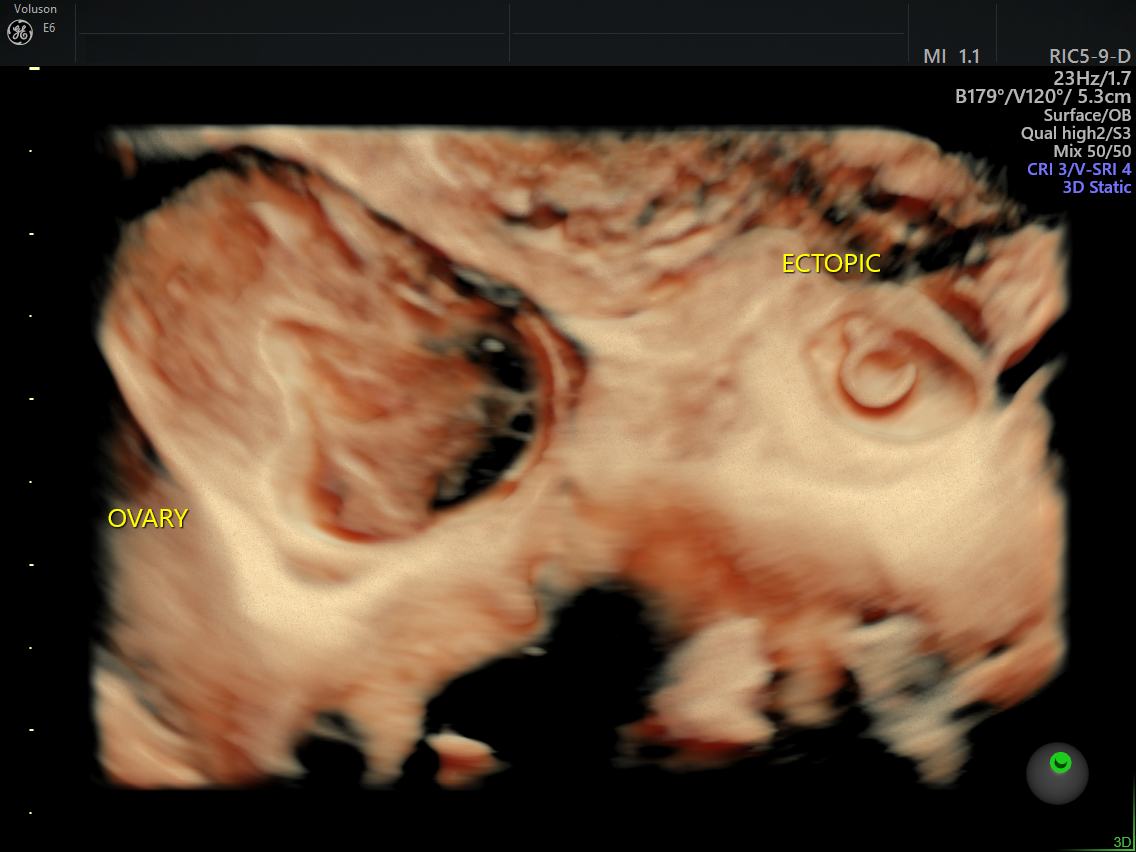
3D ultrasound of ectopic pregnancy
Providers should be familiar with various sonographic findings that could indicate specific gynecological problems. For instance, awareness of the common sonographic findings of normal intrauterine pregnancies helps you rule out ectopic pregnancies, according to research published in Applied Radiology. Hemorrhagic cysts may appear variable, and evidence of ovarian torsion may manifest as unilateral ovarian enlargement with displacement to the midline and superior to the uterine fundus.
Determining the cause of pelvic pain is not an easy task. Following specific steps, including obtaining a medical history, performing a physical examination and ordering laboratory tests and imaging studies is key to arriving at an accurate diagnosis, especially when you suspect the problem is gynecological in nature.
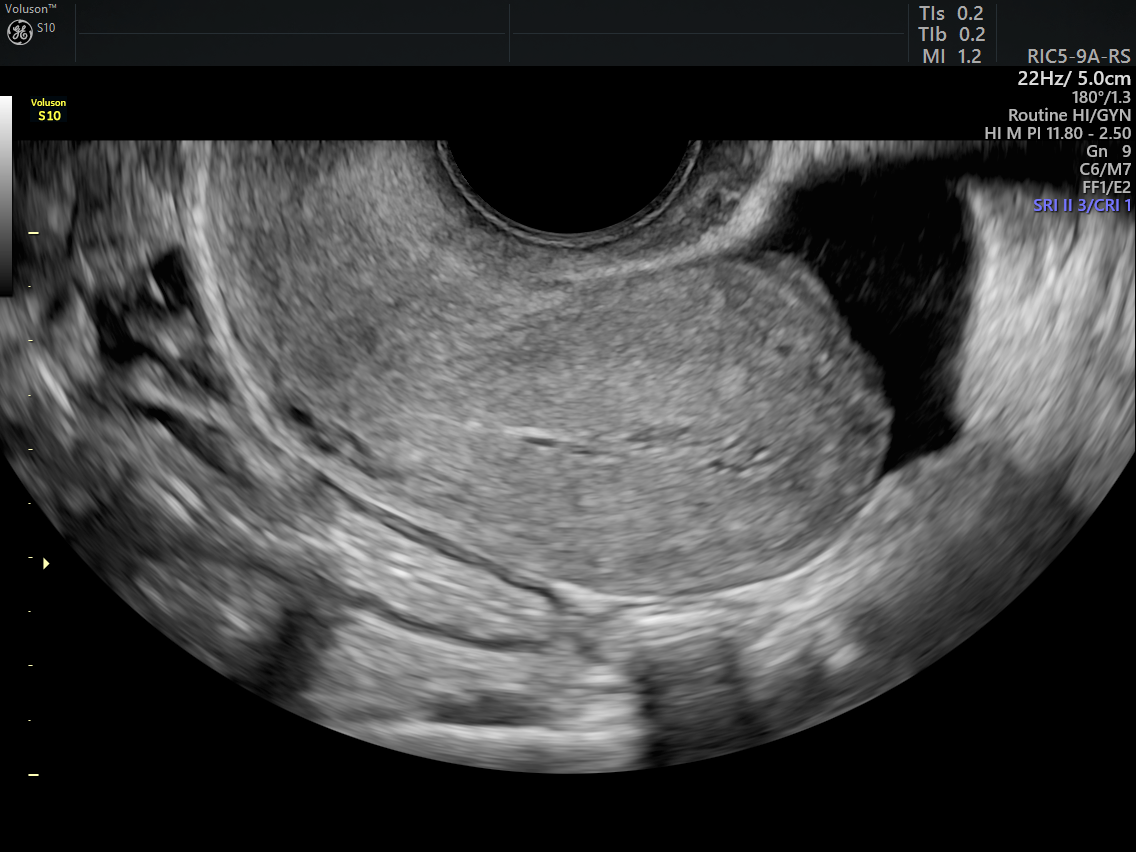
2D image showing free fluid in the pelvis
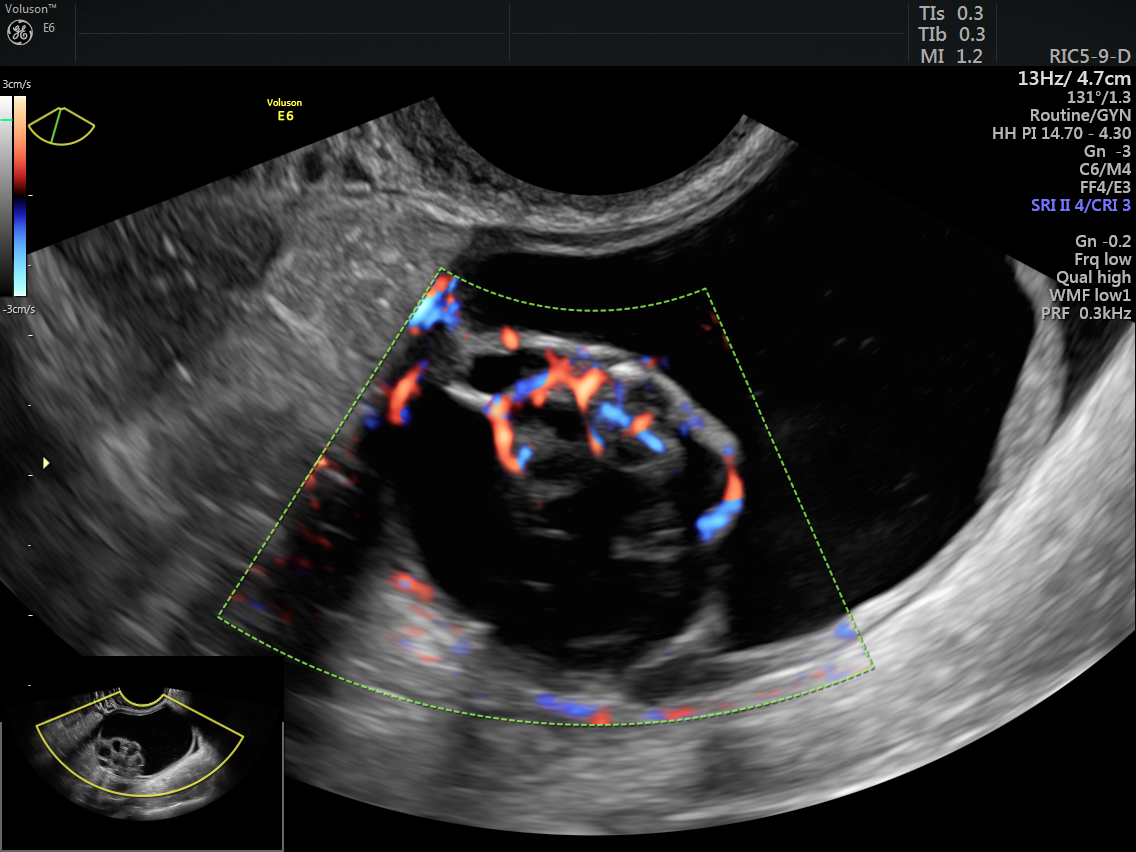
evaluation of adnexal mass with 2D and color Doppler




