Patients who are trying to conceive almost always have lots of questions for their OB/GYN. Reassurance may calm some of their worries, but many will press for concrete evidence about the state of their fertility.
A prepregnancy screening is a valuable tool not only to allay your patients' fertility concerns, but also to lay the groundwork for better health for every pregnant patient.
Steps in a Pre-Pregnancy Screening
In a joint committee opinion on prepregnancy care, the American College of Obstetricians and Gynecologists (ACOG) and American Society for Reproductive Medicine (ASRM) offer guidance on health aspects to consider in prepregnancy counseling. As the two organizations note, a prepregnancy evaluation emphasizes dual objectives — education and screening — to promote better outcomes in pregnant patients.
While a prepregnancy evaluation can include some of the hallmarks of a basic OB/GYN visit, such as a cervical cancer screening and a complete gynecologic history, the committee's guidelines further recommend taking a menstrual history to aid in assessing your patient's ovulatory function.
Most ovulatory women menstruate every 25 to 35 days, but 37 percent of women with normal menstrual cycles may be anovulatory, according to a population-based study published in PLoS One .
Consider using ultrasound to confirm ovulation, along with bloodwork such as assessing progesterone levels, if your patient's history suggests anovulation. Anovulation may be related to hypothalamic and pituitary dysfunction, obesity or polycystic ovary syndrome, a common cause of ovulatory infertility.
ACOG and ASRM further encourage clinicians to take prepregnancy screening as an opportunity to evaluate a patient's overall health. Check for chronic medical conditions that may carry risks in pregnancy, such as high blood pressure and diabetes. Managing these conditions effectively before conception may yield better outcomes for a pregnant patient.
Review any prescription and nonprescription medications your patient takes, including dietary and vitamin supplements, to confirm they are meeting recommended daily allowances. Encourage your patient to begin a folic acid supplement if they are not taking one already.
Discuss steps your patient can take to improve overall health as well, such as making healthy food choices, being physically active, reducing stress, quitting smoking if necessary and avoiding alcohol. With a patient who has a very high or very low BMI, consider broaching the subject of maintaining a healthy weight to reduce the risk of weight-related infertility and maternal and fetal risks.
Counsel on the relationship between certain STIs and fertility, and screen for gonorrhea, chlamydia and HIV if it is warranted based on your patient's age and risk factors. Chlamydia trachomatis, for example, can lead to pelvic inflammatory disease, which is one of the leading causes of tubal factor infertility, notes a report published in The Journal of Infectious Diseases.
Including genetic testing as part of screening prior to pregnancy offers the additional advantage of identifying prospective parents at risk for genetic diseases. Clinicians can offer patients and their partners education and counseling about potential prepregnancy interventions, as well as fetal testing options available during pregnancy, such as preimplantation genetic testing.
Probing for Fertility Issues
The visit may then shift to the physical aspects of reproductive health, including a targeted physical examination of the thyroid, breast and pelvic region to investigate for signs of pelvic or abdominal tenderness, organ enlargement or masses.
This stage of the visit is an ideal time to offer a baseline transvaginal ultrasound to assess the uterus and ovaries. Your patient may be reassured to learn that transvaginal ultrasound is one of the safest, most effective means of investigating many kinds of suspected pelvic pathology.
Ultrasound may reveal uterine factors associated with infertility, such as endometrial polyps and uterine fibroids. Fibroids that appear in certain areas of the uterus have a greater impact on fertility. The International Federation of Gynecology and Obstetrics (FIGO) classification system provides a well-established method for categorizing uterine fibroids and informing treatment decisions.
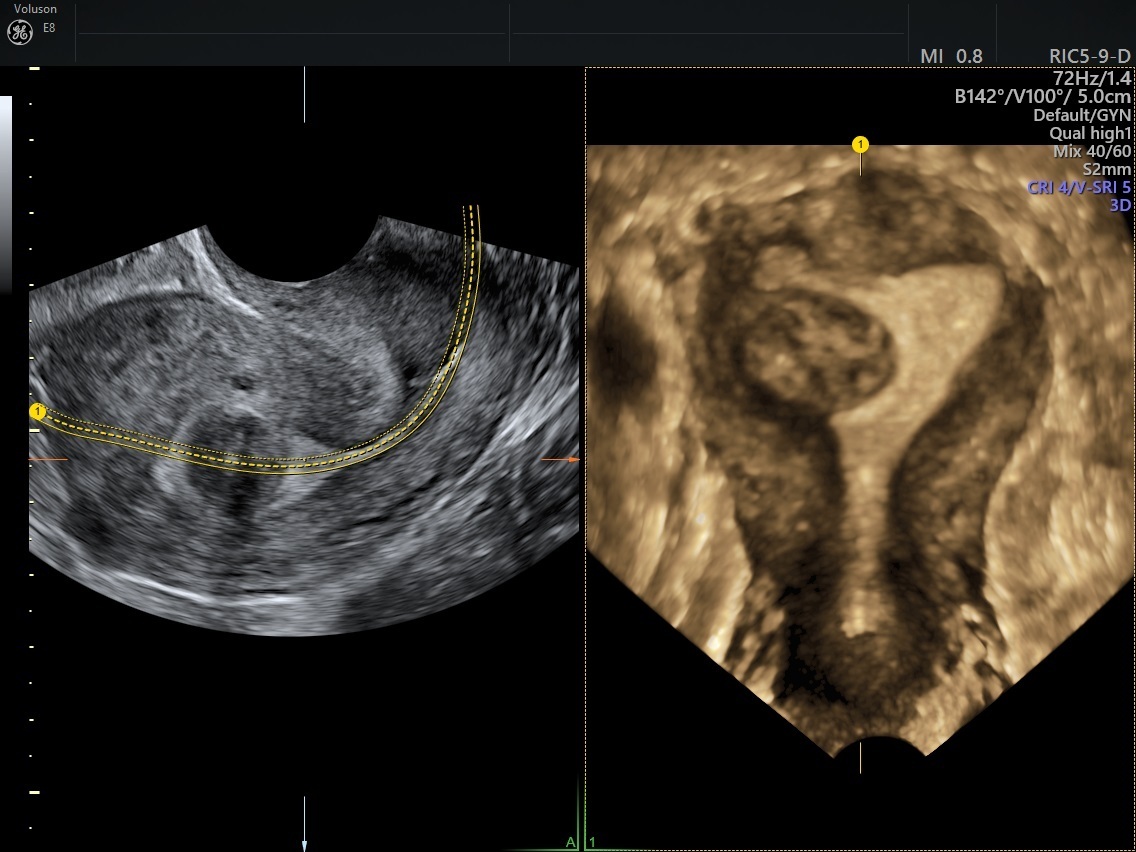
Fibroid shown with 3D ultrasound with Coronal View
For suspected endometrial polyps, transvaginal ultrasound should be used on day 10 of the menstrual cycle, when the endometrium is thinnest. Saline infusion sonography remains the gold standard for diagnosing polyps. If polyps are detected, management is guided by the type of symptoms, risk of malignancy and fertility issues. However, because most growths do not resolve on their own, surgical intervention may be required to restore fertility.
Beyond detecting abnormal growths, ultrasound is instrumental for evaluating tubal patency and ovarian function, and for estimating ovarian reserve through an antral follicle count.
Pre-pregnancy Screening Lab Work
A lab test for anti-Müllerian hormone can also provide insight into ovarian reserve. High AMH values are linked to higher conception rates, while low values are associated with lower conception rates. Ovarian reserve testing should also include an antral follicle count.
Initial lab work may include measurements of luteinizing hormone and progesterone, along with assessments of follicle-stimulating hormone and estradiol on the third day of the menstrual cycle. The information on ovulation and reproductive function that these tests reveal may suggest further avenues of inquiry.
Safely Stopping Birth Control
Before becoming pregnant, patients may ask about safely ending their use of birth control. Some might express concern about prolonged use of hormonal contraception harming their fertility.
It may help to reassure your patient that not only does hormonal birth control not affect fertility, but 83 percent of women who wish to become pregnant can do so within one year of going off most contraceptive methods, according to a meta-analysis published in Contraception and Reproductive Medicine.
As the meta-analysis notes, patients in the studies had used a wide range of methods before becoming pregnant, including progestin-only pills, combination pills, IUDs, implants and injections. The researchers found that the duration of oral contraceptive use made no significant difference in the return of fertility.
Before trying to become pregnant, patients may request the assurance of prepregnancy screening to assess their fertility. The visit provides an ideal opportunity to not only establish a foundation for a healthy pregnancy but also enrich the patient-provider relationship.


