When a patient is discovered to have retained products of conception (RPOC), the next step is not always clear. Practitioners can sometimes evacuate the tissue after a birth, miscarriage or termination without complications while preserving fertility. In other cases, intrauterine adhesions from retained material can lead to recurring issues with infertility or miscarriage. A small fraction of cases of RPOC lead to increased vascularity, which can, rarely, trigger major hemorrhages in even simple dilation and curettage procedures.
That is why, in part, the use of hysteroscopy has emerged as an alternative to curettage for patients with RPOC: This procedure helps protect the uterine cavity while reducing the risk of intrauterine adhesions and preserving fertility.
However, because hysteroscopy involves anesthesia, mild discomfort and a rare risk of permanent reproductive damage, it is not ideal as a first-line diagnostic tool for suspected RPOC but rather as an intervention for patients with a high likelihood of diagnosis.
Absent evidence-based guidelines or treatment protocols, arriving at that diagnosis requires a clinical assessment along with a combination of imaging strategies.
Clinical Assessment: Retained Products of Conception Symptoms and Risks
Patients with RPOC may present with postpartum hemorrhage as well as more nonspecific symptoms such as fever and pain in the abdomen.
Additionally, placenta accreta can raise RPOC risk, though most women will have no symptoms of that complication prenatally. Uterine scarring from previous cesarean section deliveries, placenta previa and a maternal age over 35 can contribute to placenta accreta.
RPOC on Ultrasound: What to Look for When Diagnosing Retained Products of Conception
For imaging confirmation, advanced 2D and 3D ultrasound and color Doppler can help clinicians better distinguish between RPOC and normal postpartum bleeding. Color Doppler allows clinicians to easily and quickly visualize blood flow. Added ultrasound features such as the SlowflowHD can help depict flow in vessels with low-velocity flow.
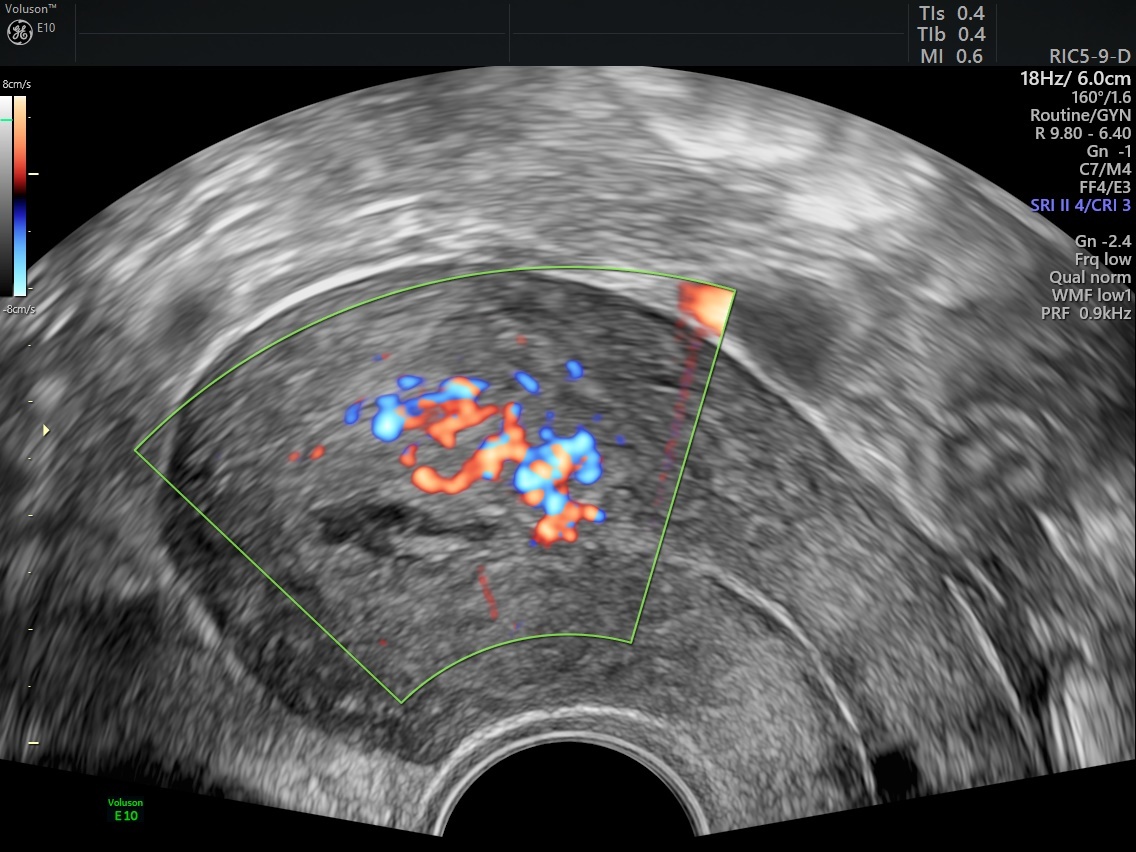
Ultrasound image showing increased vascularity suggestive of retained products of conception
Indicators of retained products of conception via ultrasound may include a thickened endometrial echo complex (EEC). The clinical threshold for a thickened EEC ranges from 8 to 13 mm, reports a study published in RadioGraphics. Clinicians should also look for signs of any endometrial masses on ultrasound and examine the vascularity through color Doppler if the option is available. It can also help to compare endometrial vascularity with the myometrial vascularity of the same image section.
3D ultrasound is preferable for examining the lining of the uterus because of the detailed view it provides of the coronal plane, notes Dr. Lawrence Platt of the Center for Fetal Medicine and Women's Ultrasound in Los Angeles. On 3D, "you can see the thickness of the endometrial lining, which you can expect to be thinning in the days and weeks after delivery. If you see large echoes filling the endometrial cavity — not just blood — you know there's a problem."
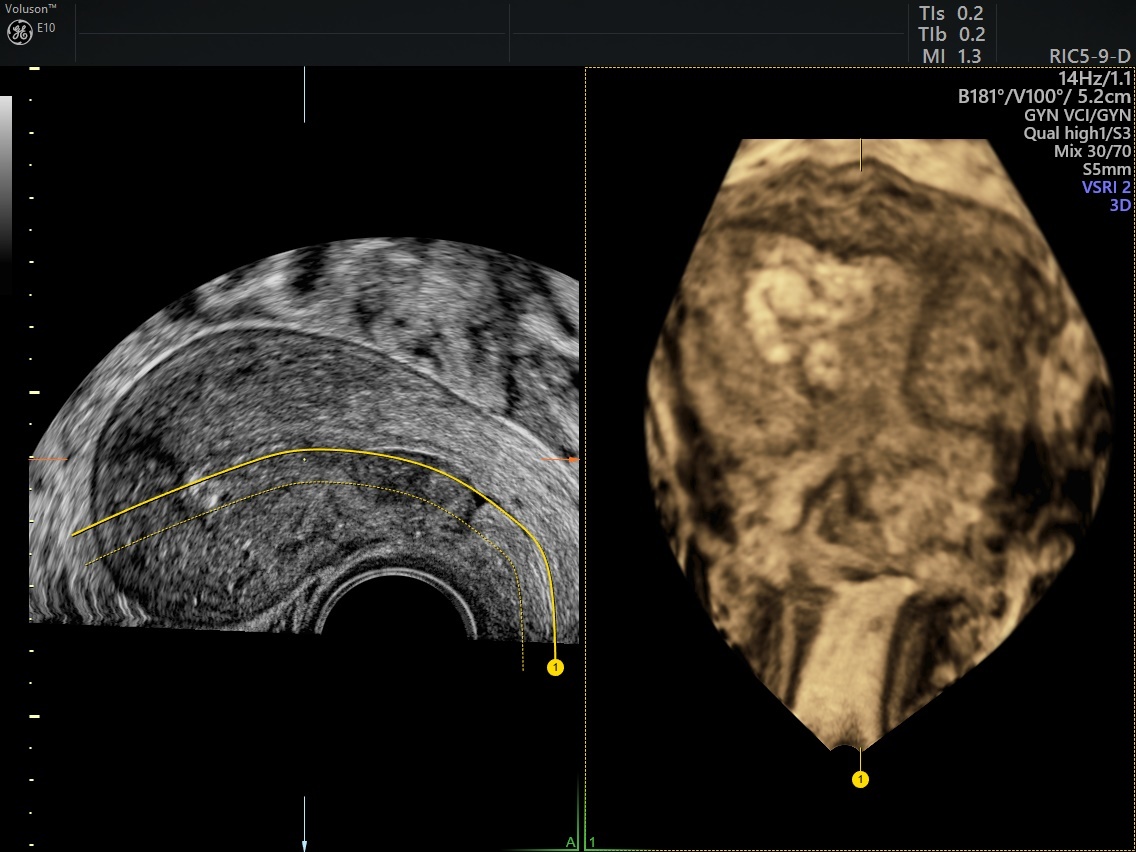
3D Ultrasound Image (OmniView) Illustrating Retained Products of Conception
If the ultrasound shows a high likelihood of RPOC, opt for immediate intervention. If it shows only a moderate risk, a provider should conduct a follow-up ultrasound exam about six weeks after delivery.
Protecting Patients and Future Pregnancies
Given the time-sensitive nature and potential fertility impact of RPOC, early detection and intervention are critical. It is imperative for clinicians to perform an ultrasound if they suspect RPOC as a cause of postpartum bleeding in order to prevent infection, adhesions and scarring, which can all lead to infertility and recurrent pregnancy loss.
"When you suspect RPOC, do you want to rush to go do a dilation and curettage?" Dr. Platt asks. The answer is no. "The risk of perforation and the risk of complications are much greater. By doing these diagnostic tests, you can reduce the risk to the patient."
A complete diagnosis and swift intervention not only protect the health of the patient but can also improve their chances for future healthy pregnancies.


