Hydrosalpinx, a dilated and fluid-filled fallopian tube, is a severe manifestation of tubal disease. It can be caused by any irritant, such as pelvic inflammatory disease (PID), a ruptured appendix, tubal adhesions from a previous surgery or endometrial deposits. Symptoms of hydrosalpinges can include lower abdominal or pelvic pain, infertility, and in some rare cases, vaginal discharge.
A speedy method of diagnosis and hydrosalpinx treatment is crucial for good patient care, as a report from Human Reproduction notes that hydrosalpinges and in vitro fertilization (IVF) have been linked. Up to 30 percent of women undergoing IVF have existing hydrosalpinges.
Methods for Diagnosing Hydrosalpinges
A hydrosalpinx is usually diagnosed after a hysterosalpingogram, laparoscopy surgery, pelvic MRI scan or transvaginal ultrasound. When a first-line, in-office assessment is needed, most of these options can be impractical. How can a practitioner be sure that they are making the best choice of modalities for their patients to ensure timely hydrosalpinx treatment?
Hysterosalpingogram uses a dye inserted via the cervix that is captured by an X-ray as it moves up to effectively paint a picture of the interior of the uterus and fallopian tubes. There may be side effects — such as pain and cramping — after this procedure, and radiation is used.
Laparoscopic surgery can also be used to see the fallopian tubes by inserting a lighted camera into the pelvic cavity via a small incision. This procedure requires general anesthesia. Seeing as it is invasive, this is not used for an initial diagnosis, but can be useful when other imaging methods reveal inconclusive results.
Pelvic MRI is able to characterize and localize adnexal masses as the dilated fallopian tube will demonstrate fluid signal intensity and incomplete folds can be seen. However, MRI is an expensive and less accessible exam that is not as suitable for everyday practices, such as with infertility assessments.
Pelvic ultrasound and the newer upgrades of 3D transvaginal imaging use the three orthogonal planes and a rendered mode, which can invert the image to allow for both internal and surface detail. Visible fluid collection near the ovaries may point to blocked fallopian tubes on ultrasound.
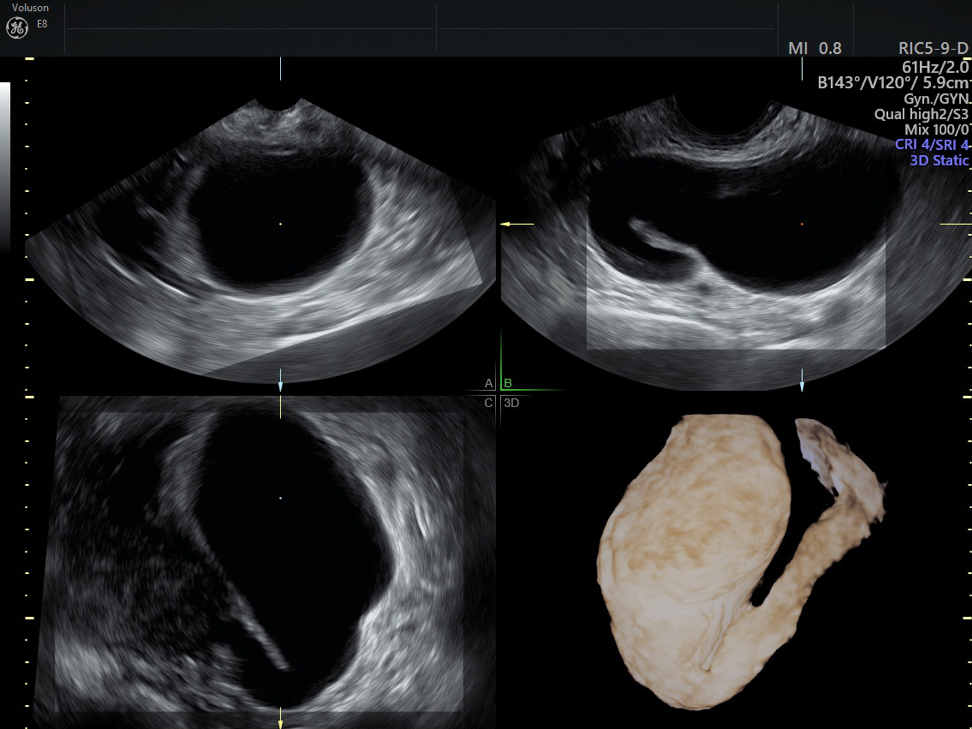
Examples of hydrosalpinx ultrasound images.
Live color Doppler provides enhanced diagnostic capability useful in the assessment of adnexal lesions such as hydrosalpinges. Edorium Journals reports that 3D ultrasound also has the advantage of real-time, surface-rendered images, where CT and MRI have limited real-time imaging abilities.
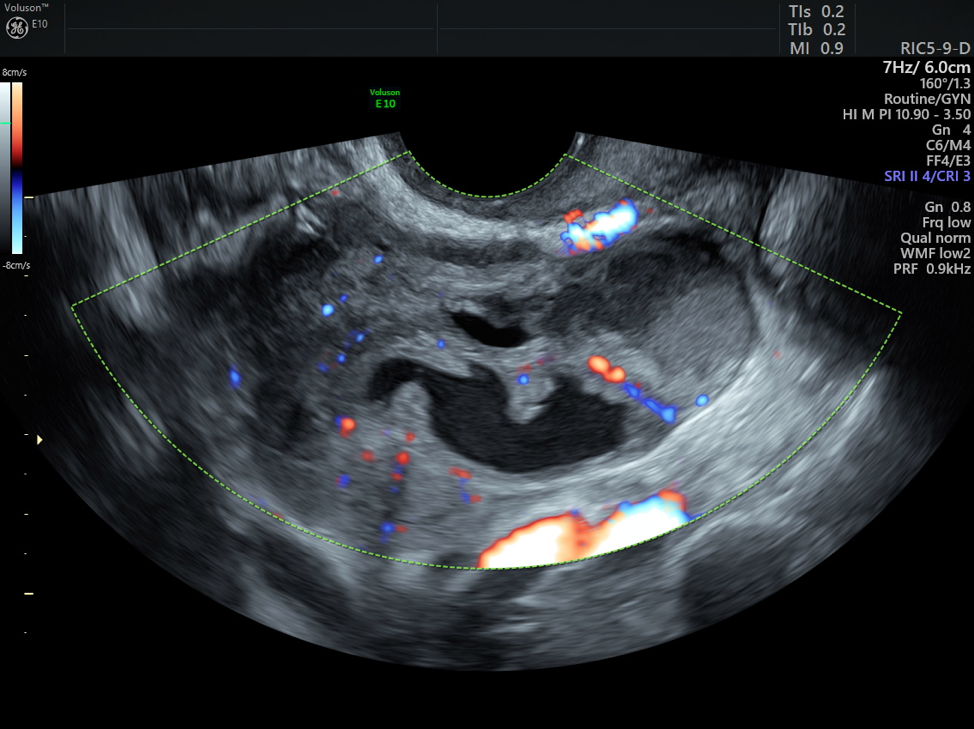
An image produced by hydrosalpinx ultrasound.
In a 2017 RSNA Session, radiologists agreed that pelvic ultrasound performs better than MRI, as long as adequate training and techniques are used. They do admit that MRI can be helpful when the ultrasound is inconclusive or if surgery is being considered, and additional information can help to either confirm or alter the treatment plan. An added benefit of 3D ultrasound is that it is radiation-free and does not require anesthesia or recovery time post-procedure.
Hydrosalpinx Ultrasound: A Faster, More Accurate Diagnosis
The imaging provided by 3D ultrasound expands the diagnostic capability of pelvic ultrasound and allows for patients to access a more comfortable, convenient and less expensive modality for dealing with pelvic pain, infertility or pre-IVF assessments. Hydrosalpinx ultrasound is one of the top options for first-line, in-office assessment of the pelvis and reproductive organs that can also ensure the best experience for your OB/GYN patients.





