Endometriosis is an ongoing, sometimes debilitating condition for patients. Now, according to Reproductive Biomedicine Online, research is finding that recurrence rates are higher than once thought — possibly as high as 50 percent, even after surgery. As awareness grows about the stubborn nature of this disease, doctors and patients should be alert to the signs of endometriosis returning. In the event that it does return, they must work together to develop a tailored plan that treats the disease as a chronic illness.
Endometriosis Recurrence
The Cleveland Clinic reports that endometriosis comes back about 20 to 40 percent of the time after conservative surgery; Reproductive Biomedicine Online places that estimate in the range of 30 to 50 percent. Both estimates may be partly attributed to an easier diagnostic process with transvaginal ultrasound, which allows doctors to recognize and diagnose recurrences sooner.
Pelvic pain and pain during sex are two of the more common signs that the disease is returning. However, your patient may have vaginal bleeding or low back pain as well depending on the location and severity of the endometrioma.
The risk of recurrence varies by the severity of the disease case and choice of surgery. For example, the disease is more likely to return if endometriomas are aspirated, and much less likely to return if the entire cyst wall is removed.
Younger patients may be more likely to choose conservative surgery if they are hoping to become pregnant in the future, making it especially important to develop an individually tailored, long-term management plan.
Preventing and Addressing Endometrioma Recurrence
How quickly can endometriosis grow back after surgery? For many women, the signs of returning endometriosis after hysterectomy or another procedure will appear about two to five years following surgery. Any post-operative management plan must be tailored to the individual patient based on their initial diagnosis, prior treatment and ongoing management strategy.
Hormonal contraceptives, which are often recommended as a primary way to manage endometriosis symptoms, have been shown to be effective in preventing recurrence. The new gonadotropin-releasing hormone (GnRH) antagonist Orilissa has also been gaining popularity for its ability to control symptoms. No matter what you or another provider prescribes, regular follow-up to discuss your patient's well-being and any possible signs of endometriosis returning should be a key part of any endometriosis care plan.
Ultrasound for Endometriosis Follow-Up
Ultrasound is the preferred imaging option for evaluating endometriosis during an initial consult, and it should be a key part of follow-up visits. Ultrasound offers a cost-effective and minimally invasive way for a clinician to ascertain the size, prevalence or potential for endometriomas.
Further surgery, including laparoscopy, is typically something that returning endometriosis patients will want to avoid. Using the information provided by transvaginal ultrasound, a gynecologist can accurately asses the need for potential surgical intervention as well as map out alternative treatment options.
Ultrasound may also provide predictive value to help avoid laparoscopy altogether. Transvaginal ultrasound, for instance, is effective at predicting the presence of endometriosis based on soft markers such as tenderness and ovary position, according to the Middle East Fertility Society Journal. Identifying these signs may allow you to create a treatment plan that anticipates and lessens the extent of endometriosis symptoms.
Although ultrasound won't prevent endometriosis from returning, it's an invaluable tool for making sure patients' needs are met throughout the course of the condition. With appropriate follow-up and an open dialogue with patients, you can develop an effective strategy to manage endometriosis as a chronic condition and ultimately reduce suffering for the people who experience it.
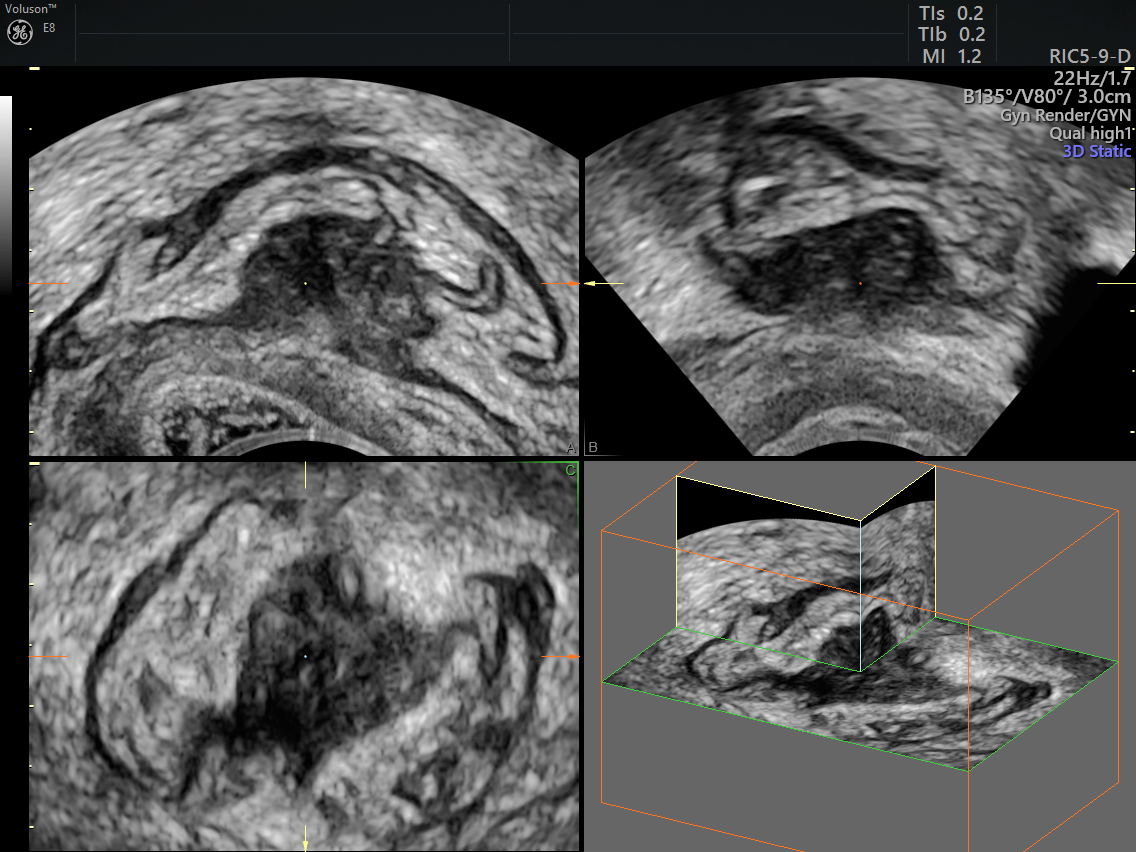
Deep Infiltrating Endometriosis using Multi Planar Reconstruction
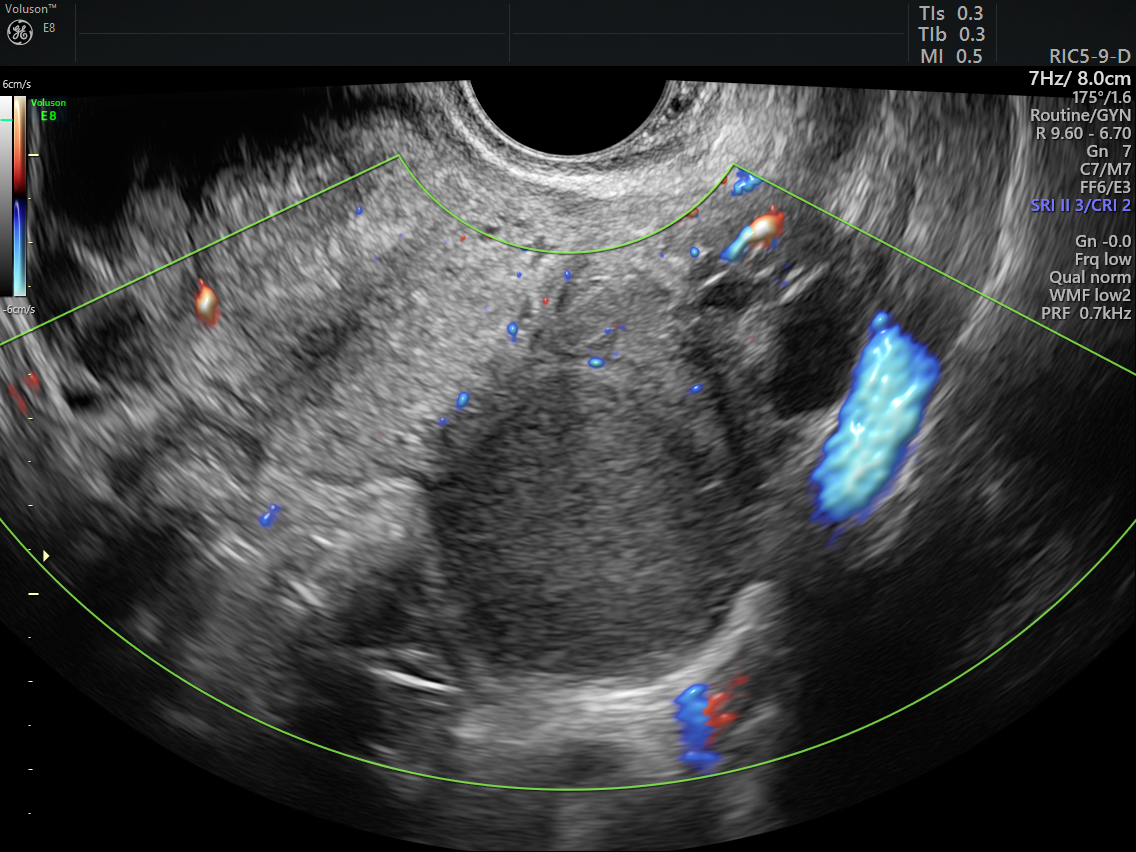
Endometrioma on an ovary





