An estimated 15 percent of heterosexual couples struggle with infertility, according to the American College of Obstetricians and Gynecologists. For patients who are unable to get pregnant within a year (for women under 35) or six months (for women over 35), an infertility evaluation is the first course of action before advancing to unexplained infertility measures.
Although infertility may appear unexplained at first, an infertility workup is likely to help identify the cause. A multidimensional process, the basic female infertility workup includes a medical history intake and physical exam paired with lab testing and imaging. This assessment helps detect problems with ovarian reserve and function, as well as the structural integrity of reproductive organs. An initial fertility workup is key for differentiating unexplained infertility from infertility with an identifiable cause, such as a tubal blockage or uterine malformation.
The Importance of Assessing Symptoms and Medical History
Understanding a patient's symptoms and medical history can provide foundational insights that begin the infertility discovery process. Symptoms can help inform next steps, including potential diagnostic tests and imaging.
There are several symptoms and prior diagnoses that should alert a reproductive specialist to a potential problem:
- Symptoms: Cycle irregularities or amenorrhea, dysmenorrhea, abnormal growth of hair on the face or body and dyspareunia, among others.
- Medical History: Pelvic inflammatory disease, endometriosis, multiple miscarriages, sexually transmitted infections, cancer or previous abdominal surgery.
However, even patients without symptoms or red flags in their clinical history can have reproductive issues. This is why ultrasound is an essential part of a comprehensive fertility workup, helping to identify the underlying factors of infertility.
Causes of infertility can range from structural problems of the reproductive organs to limited ovarian reserve or ovulatory function. Treatment depends on the specific underlying issues, but often, ultrasound is necessary for monitoring and managing infertility.
Ovulatory Disorders
Common causes of infertility fall into several key areas. The first is ovulatory disorders. Ovulatory dysfunction can lead to sporadic or stopped ovulation. A common cause of infertility, ovulation disorders can arise from hormonal imbalances or other etiologies.
Polycystic ovary syndrome (PCOS) is the top cause of ovulatory-related infertility, affecting approximately 4 to 5 million women in the United States. Though pelvic imaging should be used in conjunction with lab testing to properly diagnose PCOS, the presence of polycystic ovaries can indicate the possibility of PCOS and prompt further investigation. Other symptoms may include hair on the face and body, severe acne or an irregular menstrual cycle.
According to a consensus opinion from RadioGraphics, a polycystic ovary may present with either a) 12 or more follicles measuring 2-9 mm in diameter, or b) an ovarian volume exceeding 10 cm3. Transvaginal ultrasound can detect abnormalities and subsequently be used to monitor any ovarian stimulation.
Follicles seen using Voluson SonoAVC™follicle
Scarring, inflammation, fibroids and other problems with the uterus or cervix can affect the implantation of a fertilized egg or otherwise lead to miscarriage. Many of these conditions are common and easily visualized with ultrasound.
Endometriosis can affect fertility in several ways beyond problems with endometrial thickness, from causing tubal blockages to impacting ovulatory function. In all, up to half of patients with endometriosis experience fertility issues — and although endometriosis is not always symptomatic, patients can present with pelvic pain, dyspareunia and amenorrhea.
Through both transvaginal 3D ultrasound and saline infusion sonography, practitioners can spot abnormalities in the pelvic cavity, including adenomyosis, endometriomas and more. Surgical eradication is recommended when fertility is at stake; ultrasound can monitor treatment progress and also identify ovarian placement for in vitro fertilization (IVF) consideration.
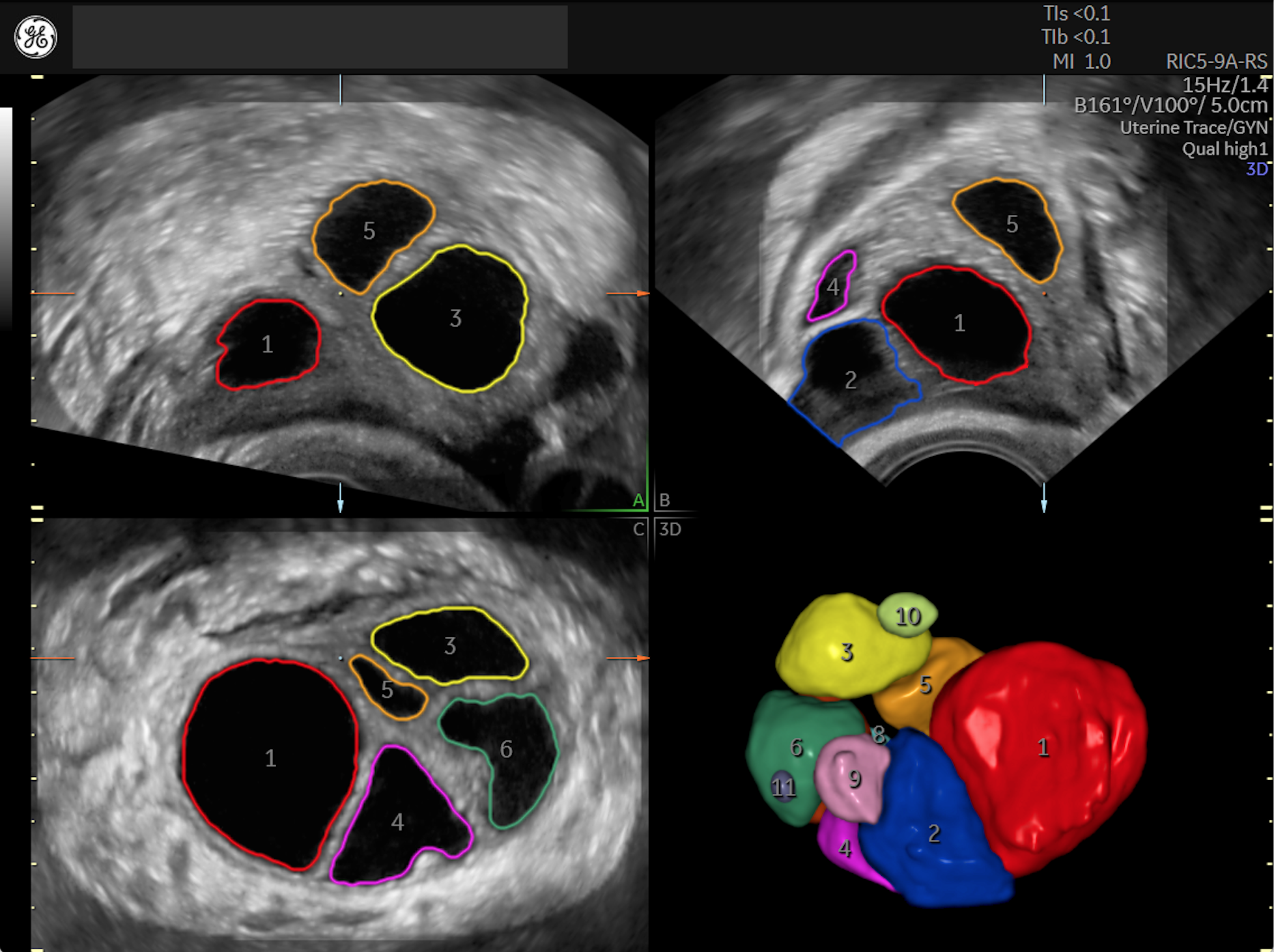
Uterine fibroids affect up to 10 percent of infertile women. They often do not cause symptoms, though they can present with cycle irregularities, pelvic pain or other signs. A fibroid's impact on infertility depends on its location, as not all fibroids in all uterine layers cause infertility. Those that do are often found in the submucosal layer as evidenced on ultrasound; these may require surgery or alternative methods such as radiofrequency ablation to preserve fertility.
3D Ultrasound of Uterus with Fibroid - using Voluson™ FibroidMapping tool.
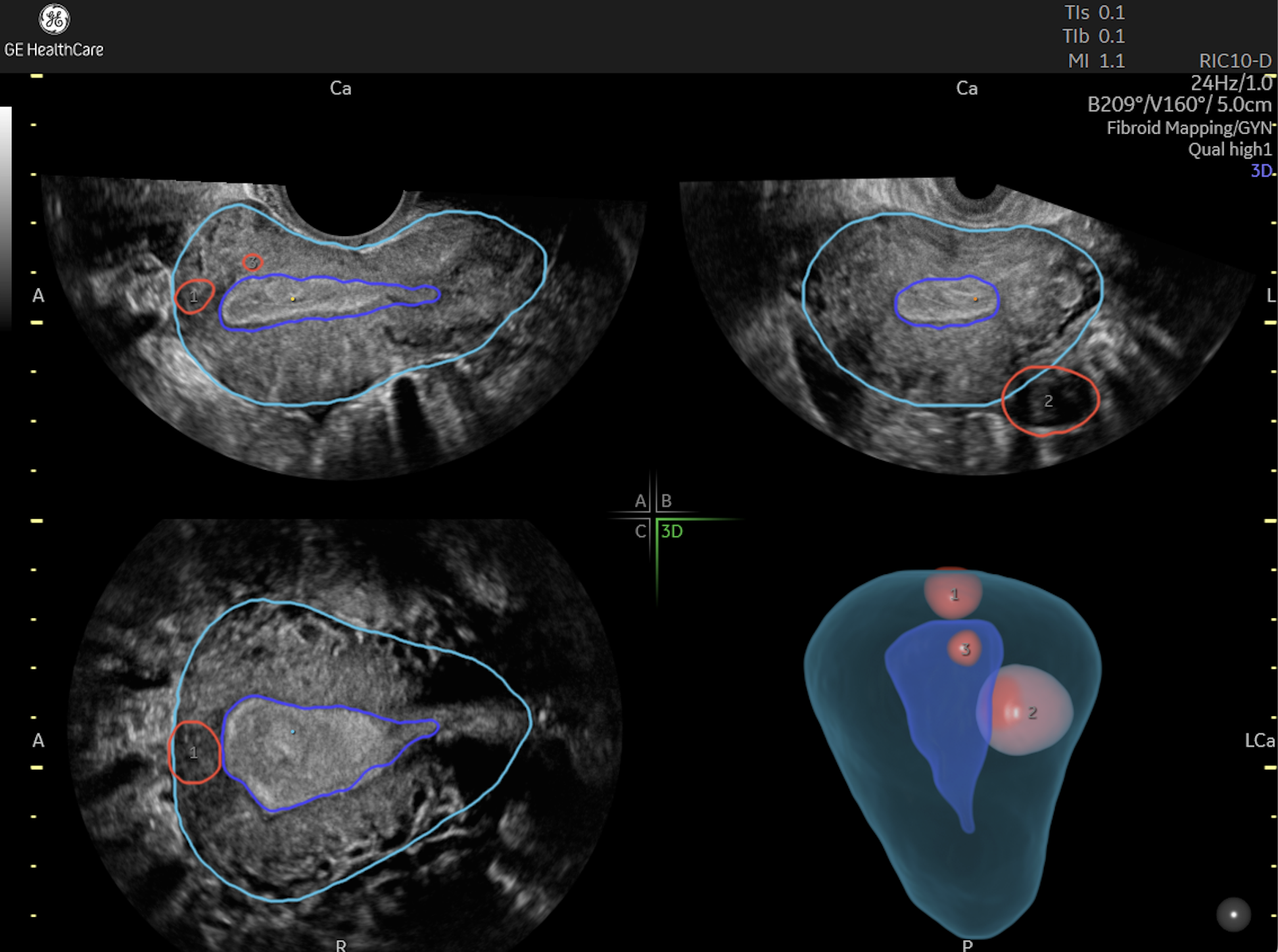
Congenital uterine anomalies are rare, but treatable, affecting 7.3 percent of infertile heterosexual couples. In contrast to acquired abnormalities such as fibroids or polyps, they are present from birth. These anomalies include the septate, bicornuate and unicornuate uterus, which impact uterine integrity, function and shape. Per guidance from the American Society for Reproductive Medicine (ASRM), 3D transvaginal ultrasound can detect and classify those abnormalities accurately and quickly. With surgery, the prognosis for pregnancy is excellent.
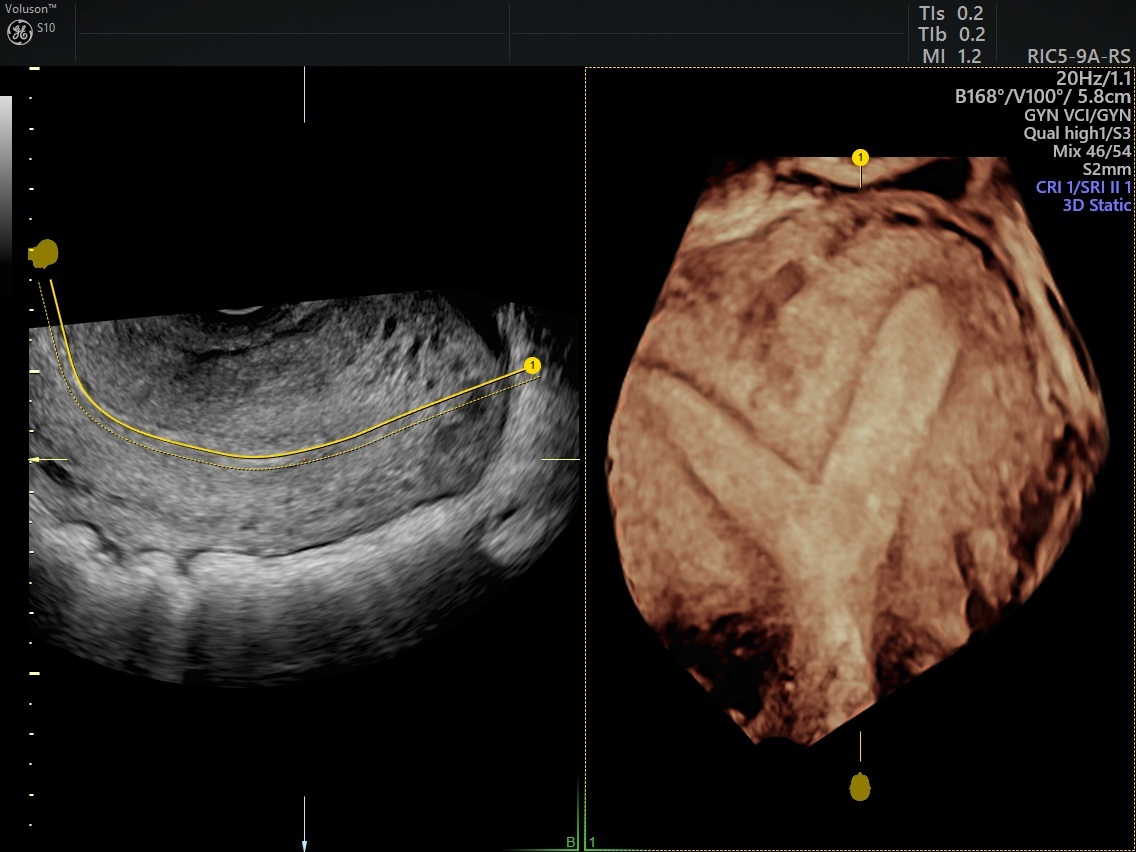
3D ultrasound showing bicornuate uterus.
Tubal Abnormalities
Structural problems with the fallopian tubes, including occlusion, peritubal adhesions and other issues, can impede egg release. These can be detected with hysterosalpingography (HSG) and 3D hysterosalpingo contrast sonography to assess tubal patency and inform treatment planning.
Tubal occlusion impacts up to 30 percent of infertile couples. This condition can be asymptomatic or cause abdominal pain. Ultrasound can play a vital role in identifying the blockage and its location, as distal tubal blockages may indicate the need for more extreme measures, such as salpingectomy or direct initiation of IVF. Patients with proximal tubal occlusions, or those near the uterus, may be able to avoid surgery with tubal cannulation. Ultrasound helps monitor treatment progress.
Sexually transmitted infections or other infections can also lead to tubal abnormalities. For example, genital tuberculosis has been linked with peritubal adhesions that affect fertility, either with mild symptoms such as menstrual irregularities or no symptoms at all. With HSG, signs of the infection are seen through edematous thickening of the tubal walls, dilatation and other abnormalities in the fallopian tubes. On ultrasound, the condition may manifest as thickened tubes or hyperechoic spots on the endometrium (indicative of fibrosis or calcification). After following the antibiotic regimen recommended by the World Health Organization, many women can spontaneously conceive post-treatment.
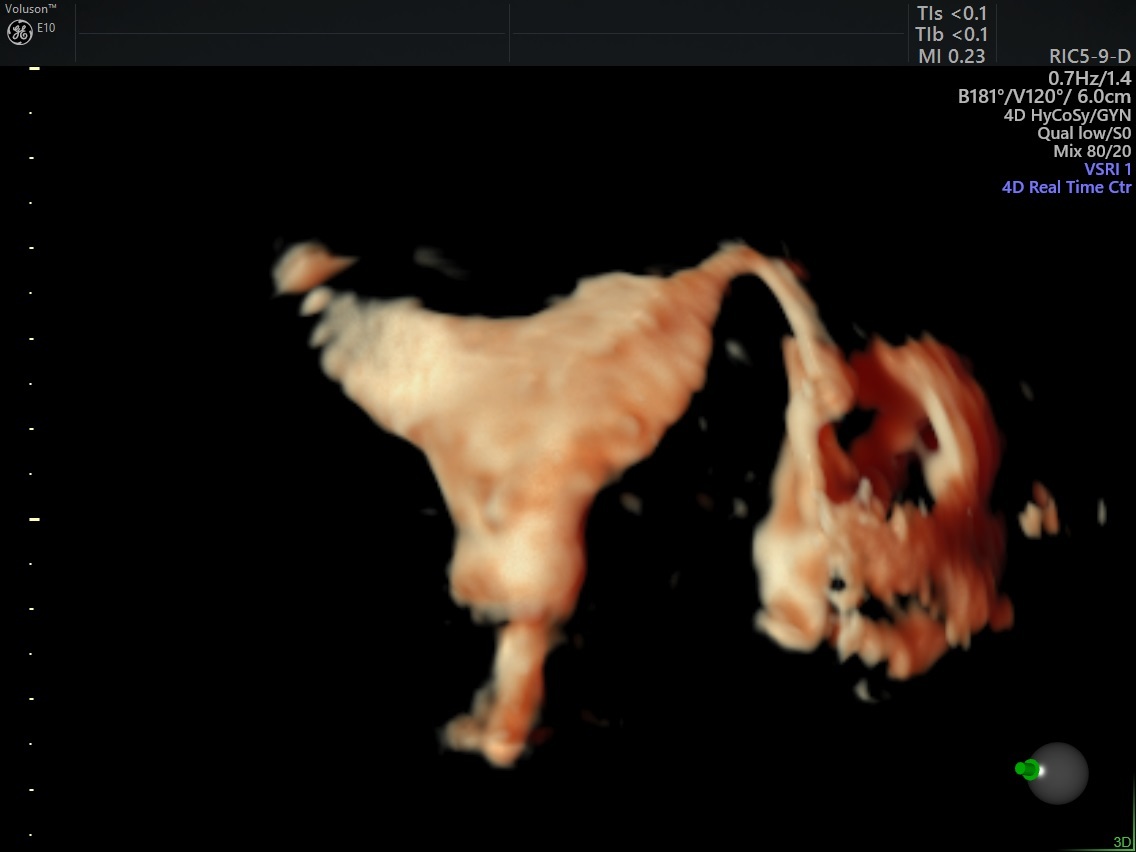
3D HyCoSy - Single Patent Fallopian Tube
Ovarian Reserve
Diminished ovarian reserve is another potential cause of infertility. By understanding the quantity of oocytes, providers can better determine a patient's potential response to stimulation for future treatments. Fewer than five to seven antral follicles can represent possible diminished reserve, as can serum measures of anti-Müllerian hormone and follicle-stimulating hormone.
Early menopause, which can affect women between the ages of 40 to 45, and premature menopause, which affects those under 40, can put a timetable to fertility and indicate the need to assess ovarian reserve. Symptoms of early menopause resemble those of menopause, including hot flashes and irregular menstruation. Transvaginal ultrasound can help quantify ovarian reserve and identify the optimal path forward.
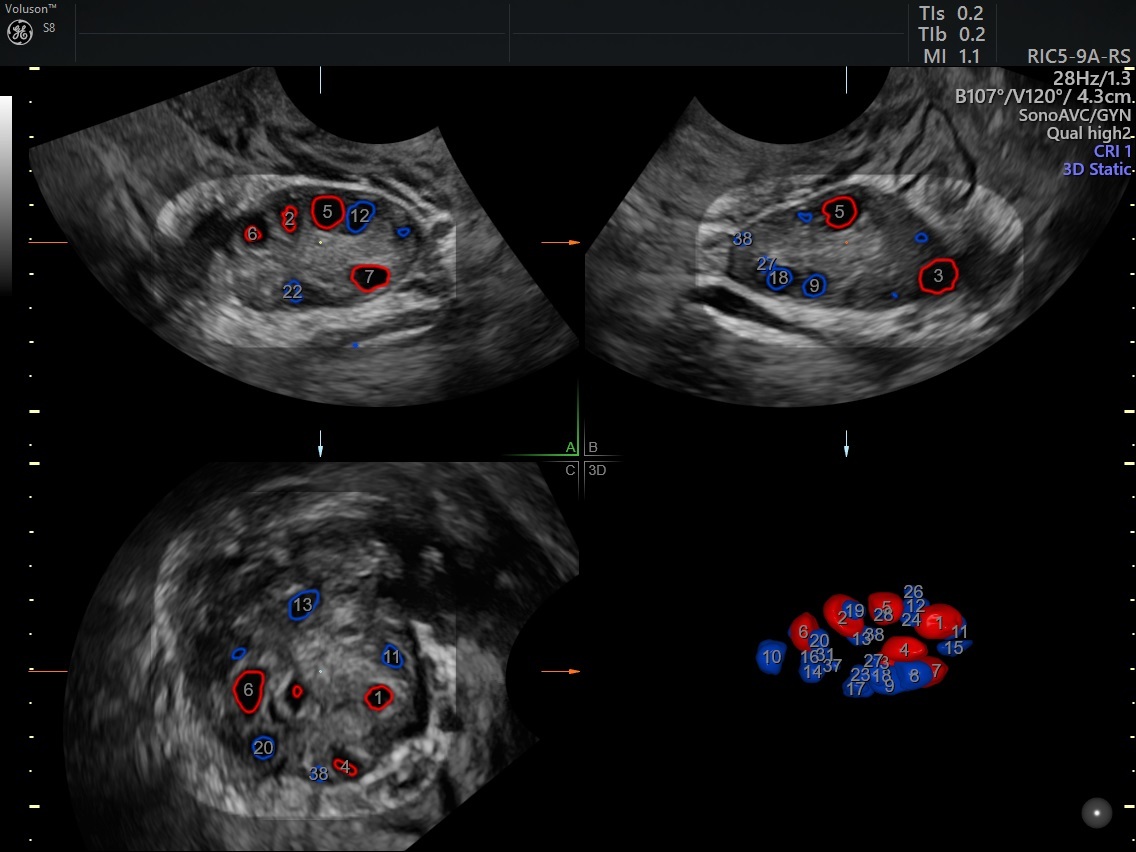
Antral follicles seen using Voluson SonoAVC™antral
Fertility and Cancer Treatment
Cancer treatments can affect fertility in different ways, such as scarring from surgical resections or ovarian dysfunctions due to chemotherapy or radiation. Ultrasound can help practitioners detect abnormalities and assess ovarian reserve. For patients of reproductive age who are interested in future pregnancy, fertility should be discussed during cancer treatment planning, including the viability of fertility-sparing surgeries.
Male Factor Infertility
A basic infertility workup should also include initial evaluation and medical history from any male partners, as male factor infertility can account for up to half of all infertile heterosexual couples. That evaluation includes taking a semen specimen, either ordered by the reproductive specialist seeing the female patient or through referral to an andrologist.
When Fertility Is Truly Unexplained
Though helpful, the basic workup is not a catch-all: Many patients with infertility may still receive normal results on all tests. When this happens, it is categorized as unexplained infertility.
Recommended treatments for unexplained infertility, as directed in guidance from the ASRM, typically start with three or four cycles of ovarian stimulation via oral medications and intrauterine insemination. If that does not yield a successful pregnancy, IVF is often the next option.
Throughout these and many other junctures of a patient's fertility journey, ultrasound can play an ongoing role. With advanced imaging, practitioners can gain comprehensive diagnostic insights that lead to more informed treatment decisions.