The purpose of a cervical cancer screening is to detect the condition early, while it is still highly treatable. The recommendations for this screening differ depending on a patient's age, but the two most common modes are the Pap test (for cytology) and HPV testing.
Cervical Cancer Screening Recommendations
The current screening recommendations from the American Cancer Society, supported by the American College of Obstetricians and Gynecologists (ACOG), are as follows:
- Ages 21-29: screening by cytology every three years
- Ages 30-65: screening by cytology and HPV testing every five years, or by cytology alone every three years
- Age 65 and over: no screening unless there is a personal history of cervical cancer, as long as most recent tests are negative
ACOG does not recommend screening for HPV in healthy women under 29 because HPV infections are normally cleared by a healthy immune system. According to the American Cancer Society, although women over 65 represent 15 percent of new cases, these women are unlikely to be diagnosed with this type of cancer if they have had regular screenings before the age of 65.
As the Journal of Clinical Medicine points out, many women have suspicious cervical cells that will never become cancerous, and more frequent screenings could lead to overuse of biopsies. Biopsy procedures such as the LEEP and conization may weaken the cervix, which is an important consideration in women of reproductive age.
Cervical Cancer Ultrasound as a Pre-Surgical Treatment Tool
If cancerous cells have been identified, the patient must receive a thorough evaluation to determine the extent of the disease. Patients may ask you, can cervical cancer be seen on ultrasound? A study published in Gynecologic Oncology compared ultrasound to MRI in assessing early-stage cervical cancer, against pathologic findings. This study found that both ultrasound and MRI were highly accurate in their pre-operative evaluations of patients, but also found that ultrasound might better assess residual tumors and parametrial invasion.
This finding was supported by a study published in Ultrasound in Obstetrics & Gynecology comparing both 2D and 3D ultrasound to MRI in assessing parametrial infiltration. The study found that both modalities of ultrasound "showed similar moderate agreement with MRI."
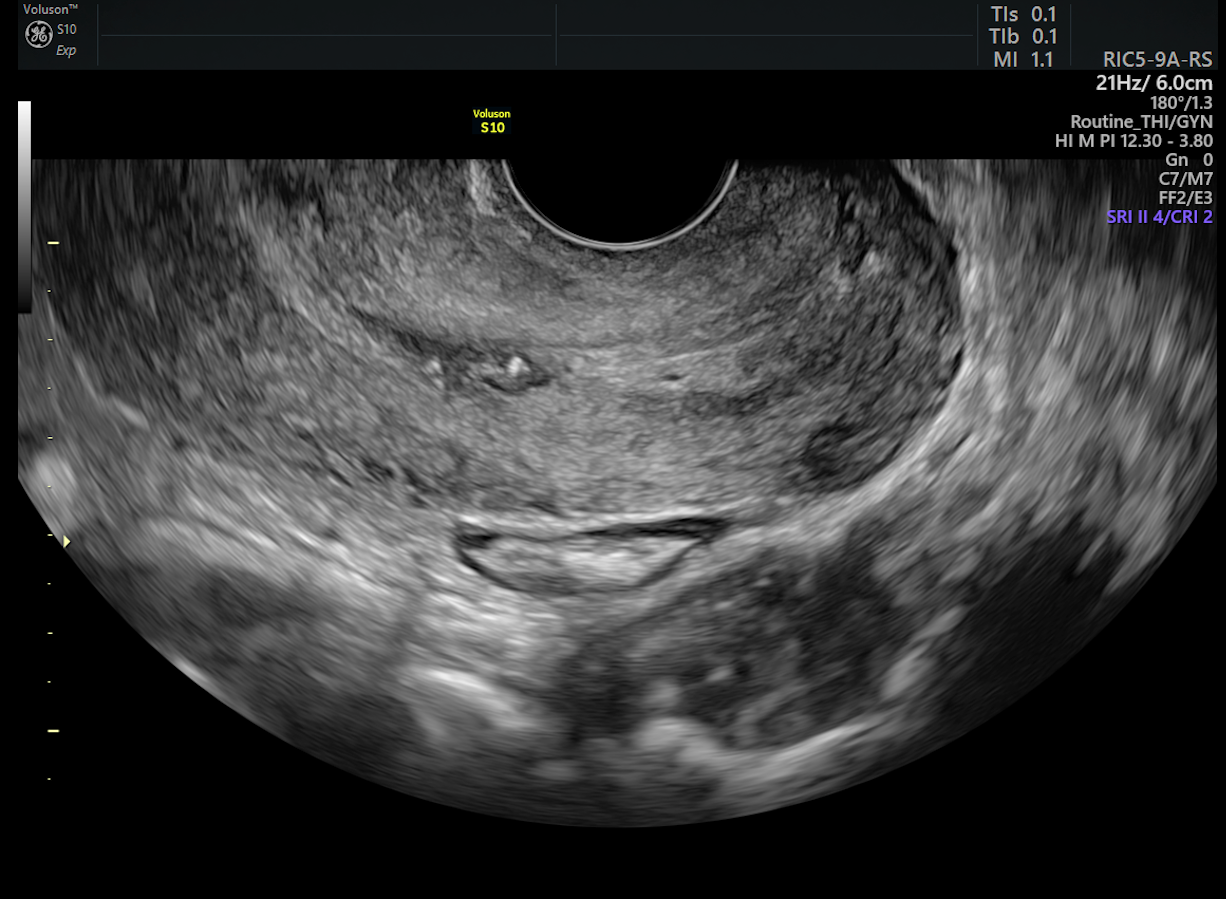
cervical cancer screening images a normal cervix
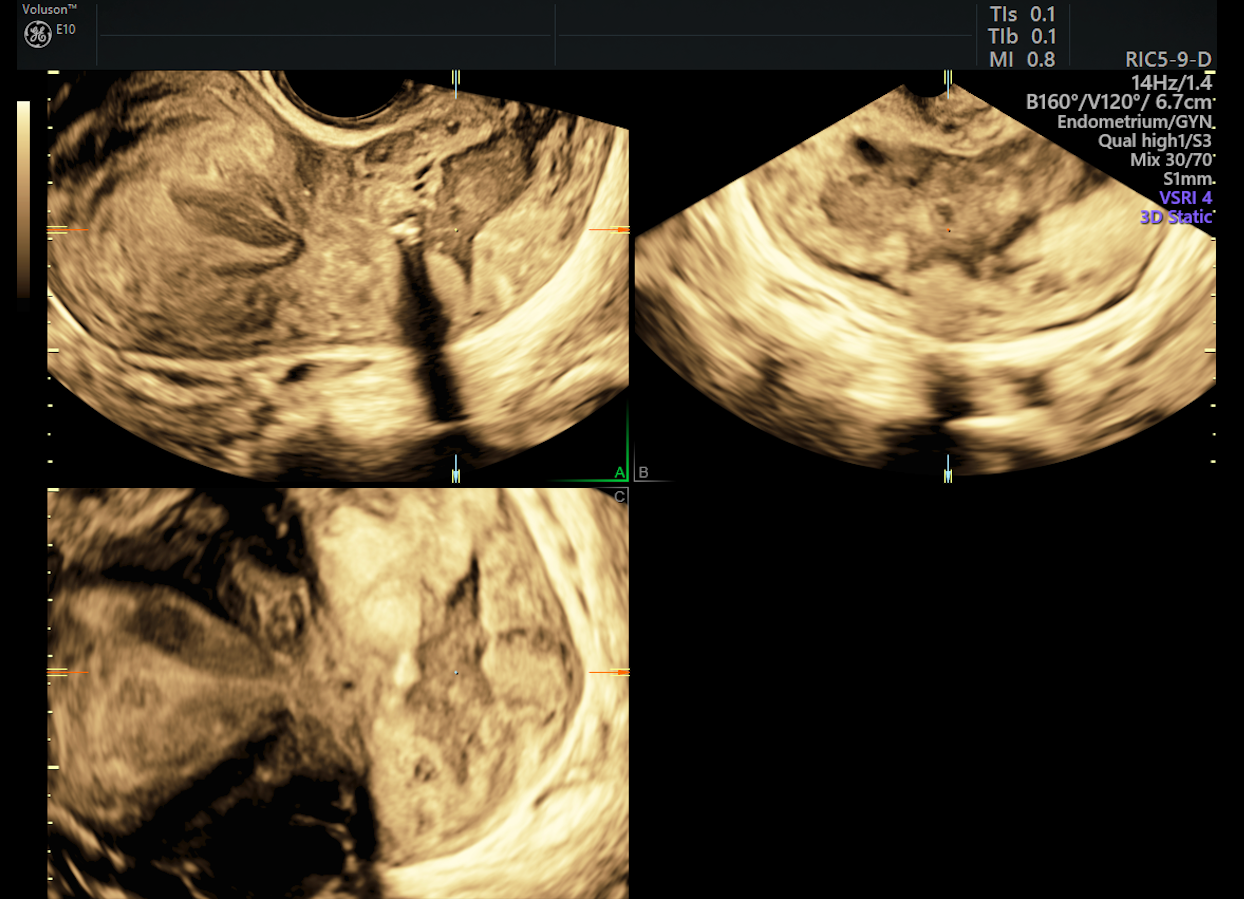
3D of advanced cervical lesion via cervical cancer ultrasound
With the addition of Doppler to 3D ultrasound imaging, a physician is able to evaluate blood flow within the cervix, as well as morphological characteristics and vascularity within masses or lesions. Yet another study comparing 3D ultrasound and MRI in the International Journal of Gynecologic Cancer states that the ultrasound is superior to MRI in assessing tumor volume and Doppler velocimetry.
If a biopsy is performed, the subsequent use of ultrasound not only allows the gynecologist to have an immediate image of the cervical and pelvic structures, but also offers a radiation-free evaluation at a lower cost to the patient.
Appropriate Uses of MRI and Ultrasound
Though it has many beneficial applications, ultrasound is not useful in identifying metastasis and cannot serve as a substitute for scans that evaluate extensive spread of the disease. As the Journal of Obstetrics and Gynecology of India notes, ultrasound is useful in identifying local disease, but it is limited in assessing lymph nodes. The use of ultrasound in cervical cancer screening, however, is one method that can eliminate the need for more invasive testing, and it provides a more comfortable and cost-effective experience for the patient.





