Uterine fibroids have a cumulative incidence of 70 to 80 percent in women under age 50, according to research from the Journal of Women's Health. Although fibroids often do not cause any symptoms, when they do, it can greatly affect a patient's quality of life.
Hysterectomy has long been the definitive treatment option for patients with fibroids, but this procedure is expensive, and comes with the risks of complications from anesthesia, postoperative complications and infection. Hysterectomy is also not an appealing option for patients who want to become pregnant. Newer treatments offer more options for fibroid management, allowing doctors to take into account the patient's preferences, quality of life and comfort, along with symptom management.
Diagnosing Fibroids With Ultrasound
Many women don't know they have fibroids unless the fibroids grow large enough to cause discomfort or other symptoms. Heavy bleeding and abdominal pain are the most common symptoms that would warrant further investigation; fibroids can also make it difficult for some women to become pregnant.
3D transvaginal ultrasound is the gold standard for diagnosing, evaluating and measuring fibroids, though transabdominal ultrasound may also be useful. Guidance from the International Journal of Women's Health notes that ultrasound is the best option because of its accuracy and availability. Plus, ultrasound is a minimally invasive exam that patients can conveniently access at their regular provider's office.
Based on how fibroids appear on the ultrasound, they are classified into three basic categories:
- Submucosal fibroids bulge into the uterine cavity.
- Intramural fibroids form on the uterine wall.
- Subserosal fibroids form on the outer surface of the uterus.
Submucosal fibroids are the most likely to cause heavy menstrual flow. Intramural fibroids can sometimes cause bleeding, but subserosal fibroids rarely do.
Fibroids are further classified according to the International Federation of Gynecology and Obstetrics (FIGO) system, or FIGO's updated PALM-COEIN system for abnormal uterine bleeding. The system classifies fibroids as types 0 through 8, depending on their size and location in the uterus. Some fibroids can be described across a range if they impact two areas; for example, a hybrid leiomyoma that is submucosal and subserosal and reaches into both the endometrial and peritoneal cavities would be listed on the PALM-COEIN chart as 2-5. A fibroid's classification is then used to determine the best treatment route. Certain types of fibroids, such as submucosal fibroids, may need to be further evaluated with hysteroscopy.
Advances in Uterine Fibroid Treatment Options
Hysterectomy remains the definitive treatment for fibroids, but that does not mean it's right for every patient. With a growing arsenal of treatment options, any fibroid management plan should take a holistic approach to the patient's health. Consider the best options to manage symptoms while balancing out the patient's feelings about surgery, as well as any desires to spare fertility or preserve the uterus.
Any management plan begins with measuring and evaluating the location and size of fibroids, since these factors may limit choices for treatment. Review the possible treatment options with your patient, and counsel them on choosing a path forward that makes the most sense for their needs.
The International Journal of Women's Health breaks down fibroid management into three categories: Medication, Surgery and Nonsurgical Procedures.
Medication
Medications are a common choice for women who have severe bleeding, but whose fibroids don't need to be removed.
- Intrauterine devices (IUD). An IUD helps reduce blood loss and can lessen anemia, but doesn't affect the size of the fibroids.
- Tranexamic acid. This medication may be given three or four days per month to lessen bleeding.
- Selective progesterone receptor modulators (SPRMs). Ulipristal acetate (UPA) is the most commonly used type of SPRM, which is an emerging option to manage fibroids. UPA decreases the fibroid volume and controls symptoms after three months of treatment. Side effects seem to be mild with this medication. Currently, UPA may be used intermittently long term, or be taken in a shorter course to decrease fibroid volume before surgery. This medication may mean the patient can have less invasive surgery or avoid surgery altogether, according to Obstetrics and Gynaecology. Research continues into the use of SPRMs, particularly UPA, to determine how they best fit into the medical management of fibroids.
- Gonadotropin-releasing hormone agonists (GnRHa). These medications that shrink fibroids are falling out of favor because of side effects like bone loss and hot flashes.
Fibroid Surgery
Surgery still remains one of the main treatments for fibroids. About 200,000 hysterectomies are performed each year to treat fibroids, according to the International Journal of Women's Health.
So far, hysterectomy is the only treatment that eliminates fibroids, but undergoing this surgery can be an emotional decision for patients. In general, it's best reserved for patients who are past child bearing age or who are not planning to become pregnant. Vaginal hysterectomy is the least invasive and least expensive option.
Ultrasound-guided hysteroscopic myomectomy is an alternative way to remove submucosal and intracavity fibroids that preserves the uterus. There is some risk to fertility with this procedure, which should be discussed with the patient in advance: Fibroids can come back, and repeated myomectomies can lead to more pelvic scarring and reduced fertility. The procedure can also be performed laparoscopically.
Nonsurgical Procedures
Advances in nonsurgical procedures also offer uterine-sparing and fertility-sparing treatments for fibroids. Ultrasound plays a key role in these procedures for accurate assessment of the location and size of fibroids, as well as excluding contraindications for some procedures. Two procedures to consider are:
- Ultrasound-guided radiofrequency ablation (RFA). This procedure decreases fibroid volume and overall uterine volume. Using ultrasound to guide the RFA device within the fibroid, the procedure uses heat to ablate the fibroid tissue. It's one of few procedures that preserves fertility while reducing bleeding and pain associated with fibroids.
- Uterine artery embolization. This procedure cuts off the blood supply to a fibroid using a catheter. While it is effective for treating symptoms related to fibroids, it is not a preferred option for women planning to become pregnant. However, it is an option for women who prefer a less invasive method and who wish to preserve the uterus.
Nonsurgical options are being used more frequently in fibroid treatment, especially in women seeking to preserve their fertility. The application of SPRMs to uterine fibroids is the biggest advancement in treatment, giving women another option to preserve the uterus and fertility with limited side effects as compared to previous treatment options.
Any fibroid management approach should consider a patient's quality of life, personal plans for pregnancy, and any desire to keep the uterus. Continued exploration of treatment options may provide even more choices to patients in the coming years.
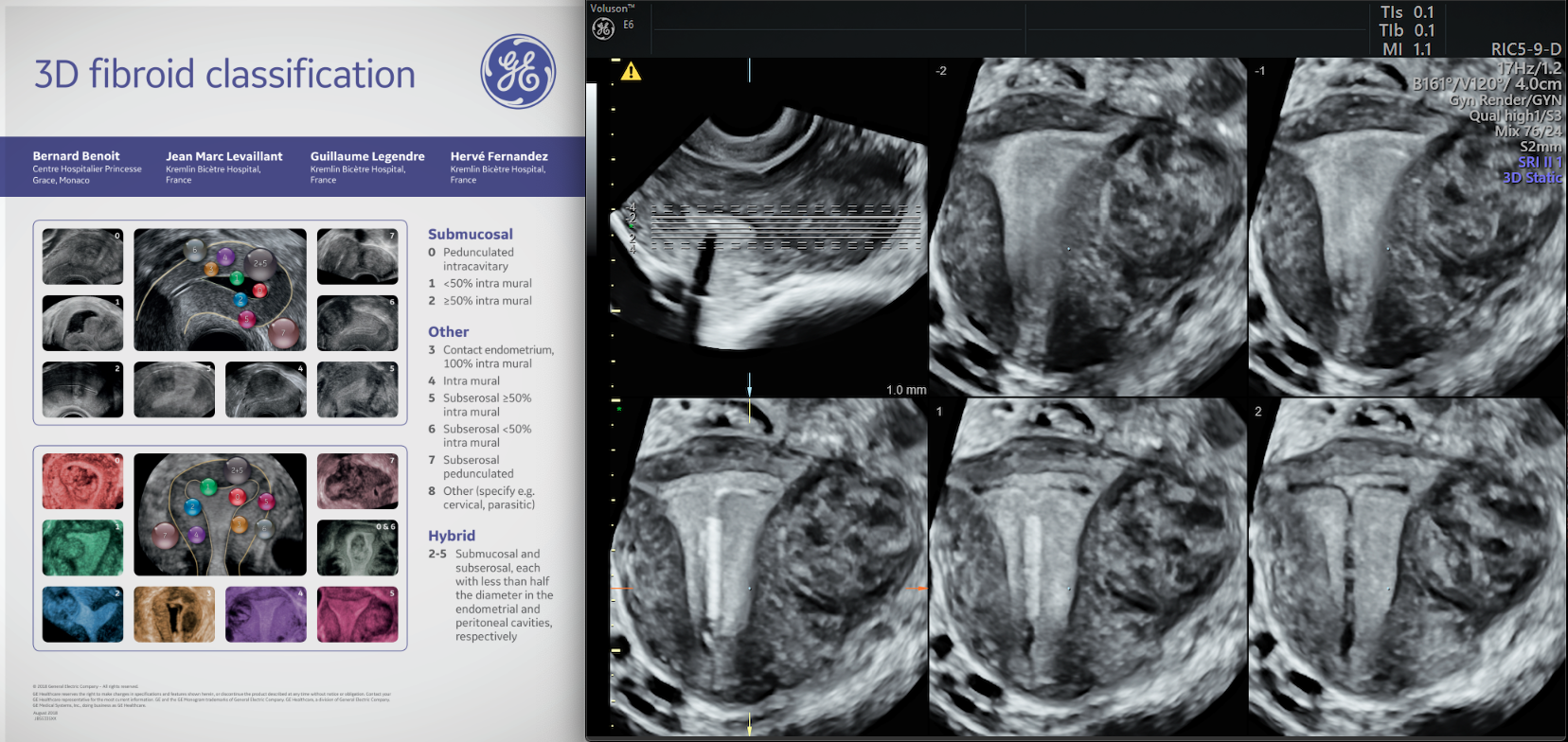
3D Fibroid classification



