Polycystic ovarian syndrome (PCOS) affects 6.6 percent or 4-5 million women in the United States, making it the most common endocrine abnormality in women of reproductive age, according to The Journal of Clinical Endocrinology & Metabolism. This condition has a variety of symptoms and contributing factors, but the key features include menstrual cycle disturbance, hyperandrogenism and obesity, which are all things to look out for with a potential PCOS diagnosis.
The health consequences of PCOS are far-ranging and include infertility, hypertension, hyperlipidemia, type 2 diabetes, coronary artery disease and cerebral vascular disease. Up to 70 percent of all PCOS patients are clinically obese, and women with PCOS are more frequently glucose intolerant or diabetic than their non-PCOS counterparts, as reported by The Journal of Clinical Endocrinology & Metabolism. They are also at greater risk for endometrial hyperplasia and carcinoma as well as breast and ovarian cancers.
Though there are many extra‐ovarian characteristics of PCOS, ovarian dysfunction is a central component, which is why accurately diagnosing PCOS should include a pelvic ultrasound for ovarian assessment.
Defining Polycystic Ovaries
Ultrasound is used to identify and document the presence of polycystic ovaries. Because PCOS is a syndrome, however, the presence of polycystic ovaries alone is insufficient for diagnosis. Therefore, pelvic imaging cannot definitively diagnose PCOS, but it does provide invaluable information during the diagnostic process.
Polycystic ovaries are commonly seen during routine ultrasounds. The Lancet Journal reports that 23 percent of women of reproductive age are likely to have polycystic ovaries. Only 5-10 percent of these women, however, will have classic symptoms of PCOS, such as infertility, amenorrhea, signs of hirsutism or obesity. Those with polycystic ovaries should not be considered to have PCOS until an additional workup is performed.
The American College of Obstetricians and Gynecologists acknowledges two criteria on the basis of which a polycystic ovary may be identified: ovarian volume and number of follicles. These criteria are based on a review of literature in RadioGraphics comparing women with PCOS with healthy control subjects. According to their consensus definition, "polycystic ovaries are present when: (a) one or both ovaries demonstrate 12 or more follicles measuring 2-9 mm in diameter, or (b) the ovarian volume exceeds 10 cm³. Only one ovary meeting either of these criteria is sufficient to establish the presence of polycystic ovaries."
It's important to note, however, that women with PCOS are frequently ovulatory. The presence of a dominant follicle (a follicle with diameters greater than 10 mm) or corpus luteum may increase the ovarian volume to more than 10 cm³. In these cases, the physician should perform additional scans during the patient's next menstrual cycle.
The Gold Standard of Ovarian Imaging
When imaging to assess for polycystic ovaries, transvaginal ultrasound is considered the gold standard due to the optimal visualization it provides of the internal structure of the ovary, particularly in obese patients. Compared with transabdominal ultrasound, it is more effective for detecting the appearance of polycystic ovaries in women with PCOS.
If transabdominal ultrasound is required — because the patient has never been sexually active or declines transvaginal examination — care should be taken that the bladder is adequately filled but not overfilled. According to RadioGraphics, an overfilled bladder can compress the ovary, "potentially leading to a greater deviation from the model of an ellipsoid used to calculate ovarian volume." The authors advise recording cine clips through the ovaries for greater accuracy in counting follicles.
With the addition of 3D ultrasound to the transvaginal routine, it is even easier to assess and image the detail needed for accurate diagnosis of PCOS. Individual follicles can be counted with certainty and complete ovarian volumes can be calculated by the software, minimizing the likelihood of an error in the PCOS ultrasound image.
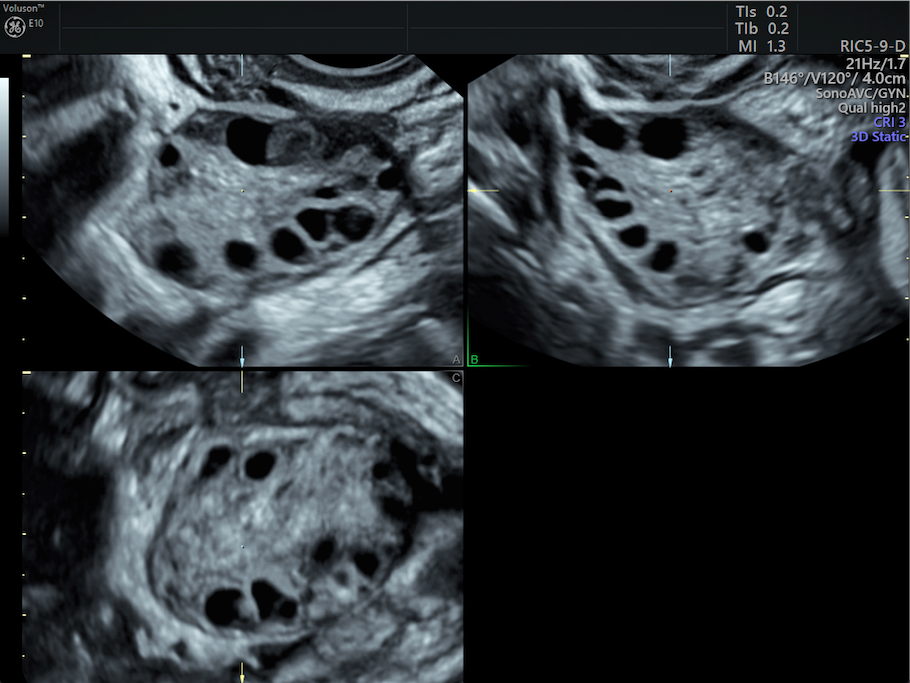
The technology makes it easy to compare ovarian sizes, and a high-resolution cine sweep makes it possible to record the ovary in real time.
Systems with image sharing tools, such as Tricefy, also enable a simple and secure connection among physicians and colleagues for collaboration, second opinions and remote viewing of necessary images for making an accurate diagnosis.
Understanding How to Diagnose PCOS
Ovarian imaging, done with the right tools, is crucial in the evaluation of patients with suspected PCOS. The imaging report should specifically include ovarian volumes, follicle counts and any other relevant information, such as the presence of a dominant follicle or corpus luteum.
Although it is common to find polycystic ovaries during routine ultrasounds, it is important to be aware of the requirements for making a PCOS diagnosis, especially if patients are being assessed for other syndromes that may signal the presence of this condition. Physicians who have the most current knowledge of clinical definitions and imaging capabilities will be able to confidently diagnose PCOS and take the appropriate next steps with their patients.