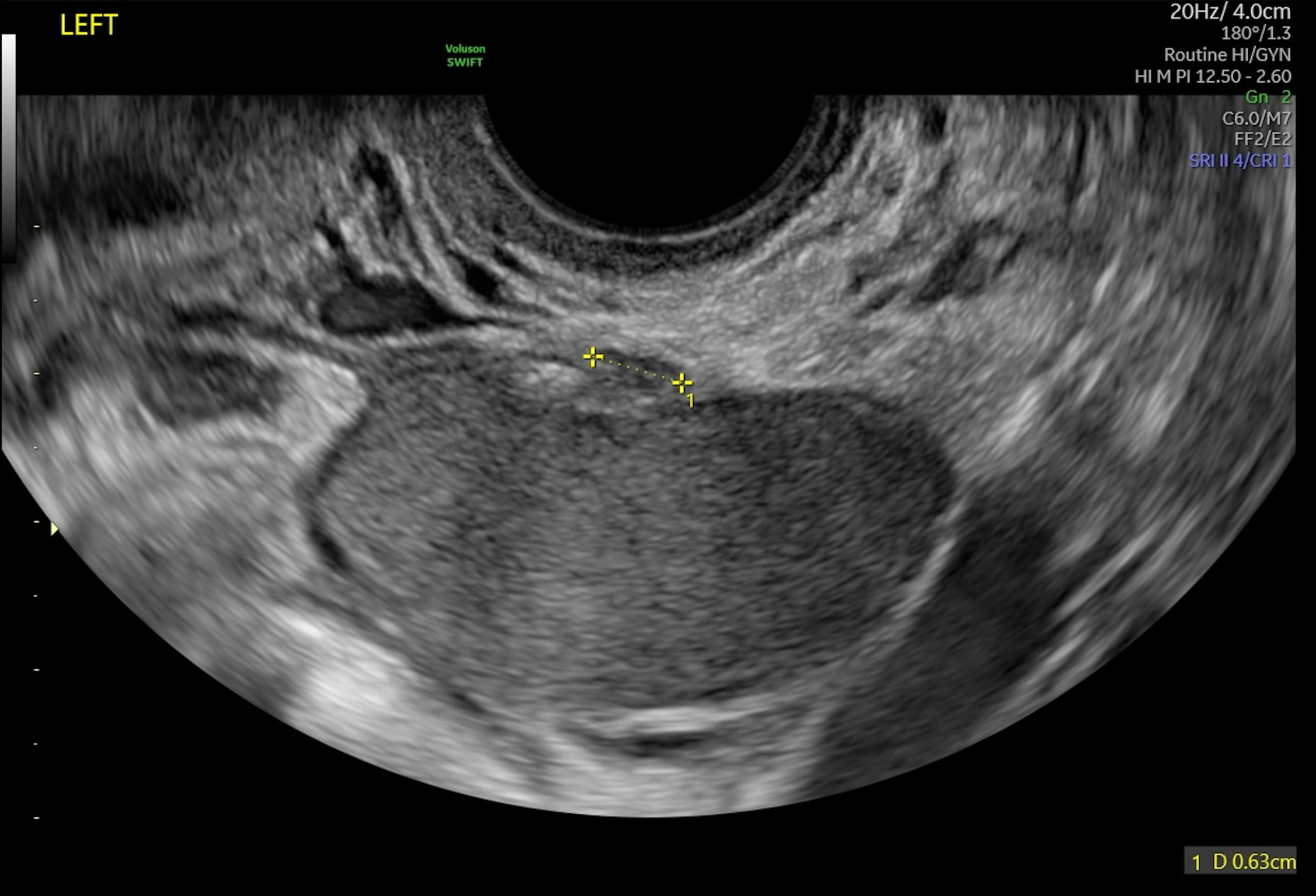
More than 11% of OB/GYN patients in the U.S. have endometriosis, a common source of pelvic pain and other debilitating symptoms that most often affects patients in their 30s and 40s.
When conservative medical management is insufficient, endometriosis surgery may relieve symptoms and help to restore fertility. Laparoscopy has long been clinicians' go-to choice to address severe symptoms or issues with fertility—but now, some are finding a new avenue to improve patients' quality of life and fertility outcomes with robotic surgery for endometriosis.
Endometriosis Standards of Care
Clinicians have historically relied on laparoscopy for the treatment of endometriosis, regardless of the severity of the disease. Laparoscopy is favored over laparotomy, as the most recent guideline for diagnosis and treatment from the European Society of Human Reproduction and Embryology explains, because it tends to provide patients with superior outcomes, such as less pain, shorter hospital stays and speedier recoveries compared to laparotomy.
Fortunately, complications from this form of endometriosis surgery are infrequent. According to a review of nearly 30,000 gynecologic laparoscopies in Human Reproduction, the risk of complications is 0.84 per 1,000 for minor laparoscopic surgery and 4.30 per 1,000 for major laparoscopic procedures, which includes treatment of moderate or severe endometriosis. The most severe complications were wound infection, adhesion formation and surgical injuries to nerves, blood vessels and other nearby structures.
Laparoscopic entry is commonly made at or through the umbilicus. That said, the abdominal wall, vagina or uterus may also serve as access points. During the procedure, the clinician carefully removes the visible areas of endometriosis, either by excision with a surgical instrument or ablation.
Visibility of the surgical field is limited, however—a problem that has led clinicians to consider the advantages of robotic-assisted endometriosis surgery in recent years. Your patient also may be curious whether this form of surgery is a better option for helping them regain fertility or quality of life.
Robotic Surgery for Endometriosis
A minimally invasive approach, robotic-assisted endometriosis surgery typically requires four to five small incisions in the midline upper abdomen, lateral lower abdomen and lateral upper abdomen. During the procedure, the surgeon is seated at a console, where they view the operative field in 3D as they carefully move robotic hand controls. The controls translate the movements of the surgeon's hands to robotic arms that wield surgical instruments.
With the advantage of high-definition 3D imaging technology, robotic surgery for endometriosis can enhance depth perception and eliminate the sensory loss common with the traditional flat view of the surgical field, according to a comparison of the two approaches published in Fertility and Sterility. Furthermore, the newer technology may improve the surgeon's dexterity, filter out hand tremors and—because the surgeon is seated during the procedure—prevent fatigue, especially during long operations.
Disadvantages include cost, lack of tactile feedback to the surgeon and a shortage of training opportunities for clinicians to learn the necessary skills to perform robotic-assisted surgery.
Beyond these pros and cons is the open question of whether robotic surgery is advisable for certain endometriosis patients more than others.
Comparable Patient Outcomes
When a multi-center research team randomly assigned endometriosis patients to either robotic-assisted surgery or laparoscopy for endometriosis, they found no differences in blood loss or complications, both during and after surgery. Furthermore, both sets of patients reported similar quality-of-life outcomes at six weeks and six months. As the authors noted, the chief difference between the two approaches was surgical time, which was about 15 minutes longer with robotic surgery.
These findings have led some researchers to investigate whether robotic surgery might offer any advantages to patients with more serious forms of endometriosis. One current avenue of inquiry is among people seeking treatment for deep infiltrating endometriosis, a complex disease that impairs fertility and quality of life.
Thus far, two recent case series suggest that robotic-assisted surgical management of deep infiltrating endometriosis may be feasible and safe.
Small Studies Yield Promising Results
Patients in a three-year case series in France published in the Journal of Gynecology, Obstetrics and Human Reproduction reported a significant decrease in pain symptoms following robotic-assisted surgery for deep infiltrating endometriosis. Major complications were rare, with only a single instance of necrosis of the right ureter five days after surgery. Of the nine patients who tried to conceive after their surgery, eight became pregnant during the study period.
Similarly, a small Italian study published in Human Reproduction found a statistically significant reduction in pain during menstruation, urination, defecation and sex following robotic treatment of colorectal endometriosis. The authors noted no complications during surgery and no major complications afterward, despite the complexity of the surgeries.
Depending on the severity of your patient's endometriosis, robotic-assisted endometriosis surgery may provide a safe, effective path to improve their quality of life and fertility. Through shared decision-making, you can make a determination that best serves your patient's health and well-being.