Staging cervical cancer is critical for clinicians to determine whether the disease has spread beyond the cervix, and if so, by how much. By accurately identifying the stage of cervical carcinoma, you can choose the most effective treatment approach.
In fact, the stage of cervical cancer is one of the most important factors in determining the effectiveness of a particular therapy, according to the American Cancer Society. Accurately staging this type of cancer requires skill — and the right tools, whether using cervical cancer ultrasound or magnetic resonance imaging (MRI).
The Staging System
When staging cervical cancer, clinicians use a scale of I to IV. Stage I means that the cervical carcinoma hasn't spread outside the uterus. By Stage IVB, the cancer has spread beyond the reproductive organs to sites such as the more distant lymph nodes, lungs, bones or liver.
Because of these distinctions, treatment for early-stage cervical carcinoma is very different from treatment for late-stage cervical cancer. For example, Stage IA cancer can usually be treated with a biopsy, while later stages may require surgery, chemotherapy, radiation or a combination of therapies.
Tools for Mapping Cancer's Growth
Traditionally, an MRI has been used to assess the size and local extent of tumors and distant metastases. However, a growing body of evidence now suggests that 3D ultrasound is equally effective at staging cervical cancer.
Transvaginal ultrasound can be used not only to detect tumors, but also to measure the size of tumors and the degree of stromal infiltration. These cervical cancer ultrasound images are also useful for examining the pelvic lymph nodes and ascertaining whether the parametrium, bladder or rectum are affected by the cancer.
A study published in the Journal of Clinical Ultrasound compared the accuracy of a transvaginal ultrasound scan with that of an MRI in the local staging of cervical cancer in 46 patients. The researchers found that both techniques had a sensitivity of 80 percent, a specificity of 50 percent and a diagnostic accuracy of 63.6 percent for the detection of stromal invasion in early‐stage cervical cancer. They concluded that transvaginal ultrasound "may be used as an adjunct to MRI for the local staging of invasive cervical cancer, or to allow for rapid and confident triage of patients into operative and non-operative categories for management in the gynecologic outpatient setting."
Potential Benefits of Ultrasound Scan Over MRI
Researchers have found that 3D ultrasound in particular is a useful alternative to MRI in staging cervical cancer. In one study of women who had either early- or advanced-stage cervical cancer, transvaginal 3D ultrasound performed as well as MRI in assessing whether the cancer had infiltrated the parametrium or spread to the bladder. Another study, from the Journal of Ultrasound in Medicine and Biology, compared both approaches and found that the accuracy of preoperative staging was 92.50 percent for transvaginal 3D ultrasound and 82.50 percent for MRI.
When staging cervical cancer, you may want to consider adding 3D ultrasound to your clinical toolbox. It's an accurate, cost-effective and simple-to-use technology that can play an important role in helping diagnose and stage this form of gynecologic cancer. An early-stage cervical cancer ultrasound and diagnosis can help your patient better plan their treatment and recovery.
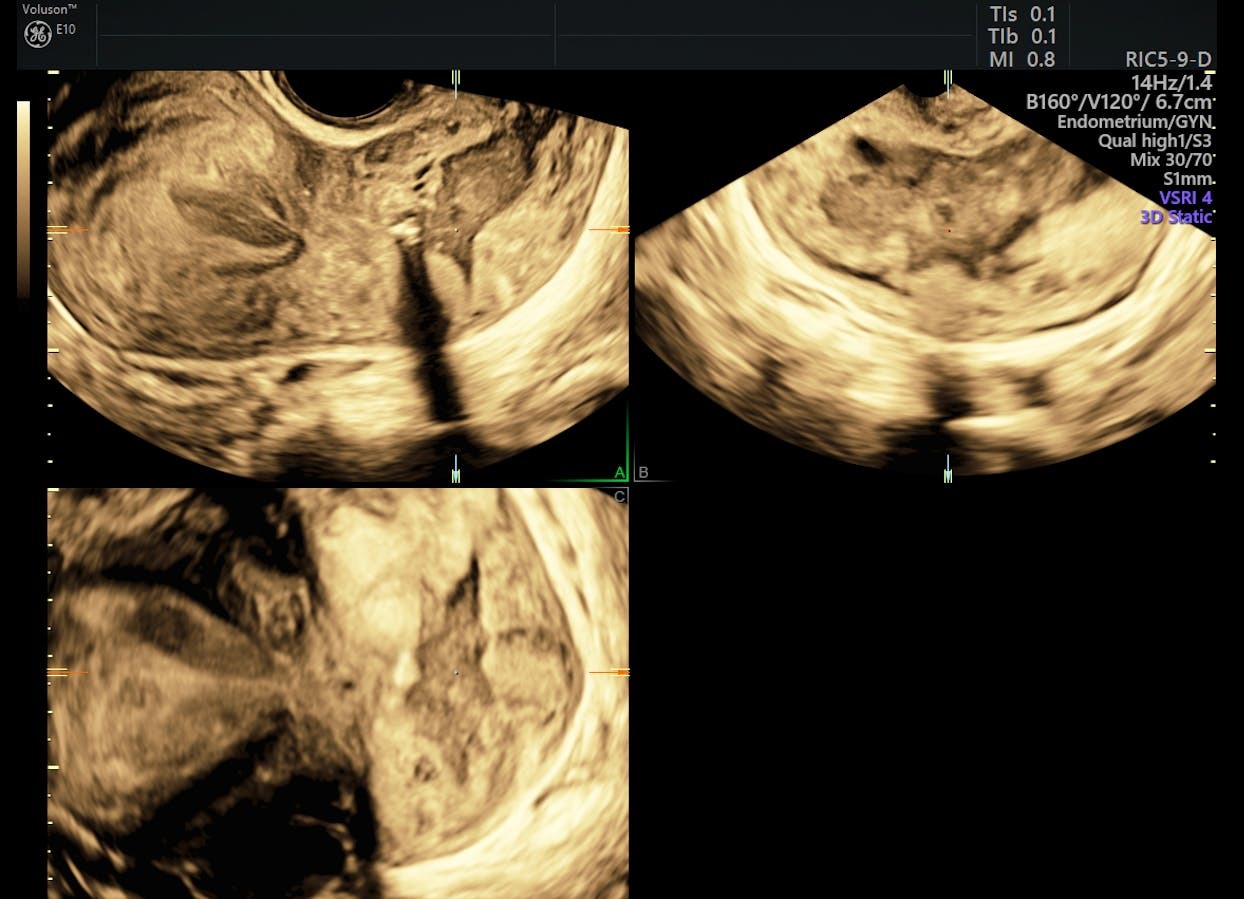
3D ultrasound of advanced cervical lesion





