Endometriosis is one of the most common diseases affecting reproductive-aged women and individuals assigned female at birth, but it can lead to a major decrease in quality of life and productivity.
Beyond the well-known experience of period pain, other types of pain — such as pain with bowel movements, pain with intercourse and chronic daily pelvic pain — can arise alongside non-pain complaints, including subfertility, bloating and bowel habit changes. For this reason, it is essential that endometriosis screening is accurate and achieved within a short time after individuals begin presenting with symptoms.
Reconsidering Laparoscopy as the Gold Standard
Thus far, clinicians have relied heavily on invasive diagnostic laparoscopy for the direct visualization of endometriosis lesions and the pathological assessment of any removed tissue. Laparoscopy is considered the gold standard method for diagnosing endometriosis. However, this can bring issues as well: Surgery is invasive, expensive and carries risk.
Importantly, diagnosing endometriosis at surgery is also not perfect — the disease may be missed or the severity of it may be underappreciated. Moreover, not all patients diagnosed with endometriosis actually require or want surgical treatment, so performing surgery for diagnosis may be excessive. Treatment options should be guided by evidence and patient preference.
How Ultrasound Helps Clinicians Assess Endometriosis
Fortunately,
, advancements in ultrasound screening have made detecting endometriosis easier than ever. Two of the three subtypes of endometriosis — ovarian endometriomas and deep endometriosis — are visible and reliably detected using ultrasound when the operator of the ultrasound machine is trained. A late-stage complication of endometriosis called obliteration of the rectouterine pouch (also known as the cul-de-sac or pouch of Douglas) can also be a reliable method of detection using the dynamic sliding sign test while performing a transvaginal ultrasound. The realization that rectouterine pouch obliteration could be visible on ultrasound helped evolve ultrasound's utility from a diagnostic tool to a surgical planning tool.
When it comes to diagnosing a problem, having different techniques available is helpful. In addition to 2D-ultrasound, 3D-ultrasound can be used to enhance the views of the pelvis to assess endometriosis. Using ultrasound, it has become possible to both predict the stage of endometriosis using the American Society of Reproductive Medicine (ASRM) classification system and to predict the complexity of endometriosis surgery using the Ultrasound-Based Endometriosis Staging System (UBESS). Ultrasound's ability to predict the stage of endometriosis and the complexity of a potential surgery allows a gynecologist to counsel the patient comprehensively and obtain informed consent for treatment options.
Using Ultrasound to Plan Surgery
If surgery is under consideration, ultrasound has the potential to be the tool that guides a surgeon on whether they have the necessary skill set to perform the surgery themselves. It is well-recognized that most graduating obstetrician-gynecologists are not comfortable with endometriosis surgery — advanced training in minimally invasive gynecologic surgery is often necessary to handle these cases. When surgery is ultimately decided, ultrasound helps surgeons determine how long the surgery might take, as well as whether they need the help of other surgeons such as colorectal or urological surgeons. This is most often the case most when bowel or bladder endometriosis is detected.
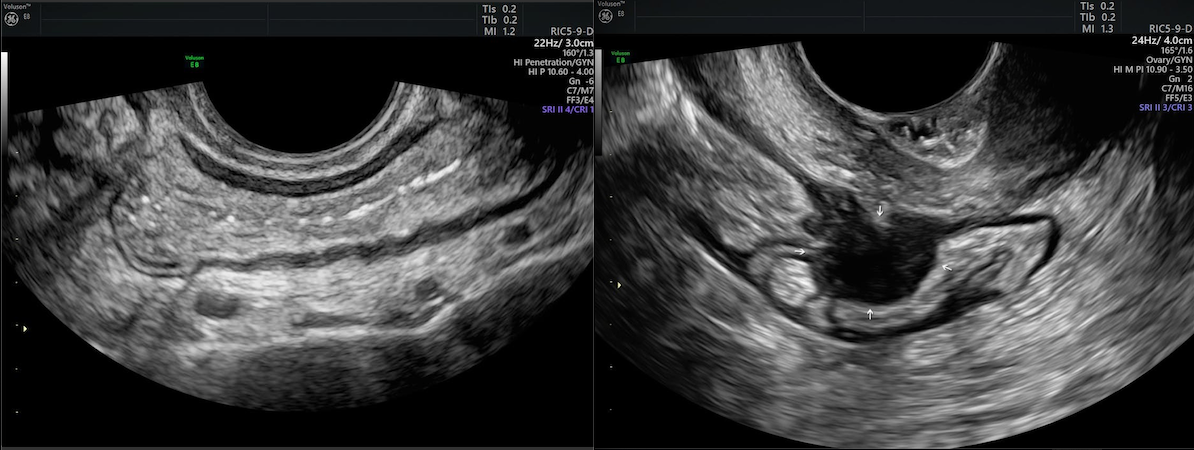
(L) 2D ultrasound of normal bowel wall. (R) 2D ultrasound of Deep Infiltrating Endometriosis (DIE) in bowel wall
While using noninvasive imaging tools like ultrasound for endometriosis screening has limitations, it has become abundantly clear that the care pathway of those concerned they have endometriosis must integrate ultrasound. In the absence of ovarian endometriomas, deep endometriosis or rectouterine pouch obliteration, superficial endometriomas may still exist. The latest ultrasound research is bringing the field closer to evaluating the pelvis for more subtle pathology such as superficial endometriosis. Research on 3D ultrasound is growing as well to demonstrate improved accuracy in detecting deep endometriosis. Ultrasound has the ability to reduce the number of individuals who undergo a two-step diagnostic and therapeutic process involving a diagnostic laparoscopy followed by excision of endometriosis through surgery. This has the potential to save the healthcare system money — but more importantly, it saves patients from unnecessary surgery and its associated risks.


