Perimenopause represents an important, and often scary, phase of patients' lives. They have not yet closed the book on their reproductive years, but have already started to experience hormonal changes. According to the National Institute on Aging, this period can last for seven years or more; during this time, perimenopausal patients commonly consult their physicians for a variety of symptoms like worrisome bleeding, hot flashes and vaginal atrophy. Routine pelvic exams may indicate other problems in asymptomatic women, such as an enlarged uterus or ovaries.
Sometimes, issues may be addressed with first-line perimenopause treatments such as hormone replacement therapy (HRT), according to research published in American Family Physician. Other times, finding the treatment is more complicated. A clinician's ability to accurately assess and diagnose issues as noninvasively as possible makes all the difference in the patient experience. Ultrasound is a critical tool for monitoring and directing patient treatment throughout perimenopause.
How Ultrasound Helps Perimenopausal Patients
Ultrasound gives clinicians real-time insights and detailed visuals. In particular, 3D ultrasound can depict the coronal plane, in addition to the sagittal and transverse planes depicted by 2D ultrasound. With onsite ultrasound, doctors can examine their patients during a single clinic visit, rather than having to wait for imaging reports from referring physician, which could result in additional imaging or clinic visits for the patient.
"There's a difference between examination by referral and examining your own patients with transvaginal ultrasound," says Dr. Steven Goldstein, a gynecologic practitioner in New York. "Every time information is passed off by someone else, there's the chance for error."
If imaging suggests abnormalities, physicians can triage interventions to expedite treatment planning. But which perimenopausal concerns call for in-clinic imaging, and how can ultrasounds help identify them?
Abnormal Uterine Bleeding
As one of the most common concerns linked with perimenopause, abnormal uterine bleeding (AUB) cannot only worry patients, it can affect their quality of life. Though instances of AUB often boil down to benign factors — such as cycle irregularities, HRT or atrophy — other causes such as endometrial hyperplasia and malignancies pose a serious concern.
Early detection is key. Dr. Lisbet Hanson recommends the noninvasive route as a first step to measure endometrial thickness and screen for endometrial hyperplasia.
"Personally, I believe doing the ultrasound first makes the most sense," she says. Many OB/GYN practices and hospitals offer ultrasound, and one routine exam can reveal any issues with the endometrium, adnexa and uterus.
As far as timing goes, Dr. Hanson advises, "Your best shot at measuring the endometrium is before it is disturbed by the biopsy. You may also detect a focal abnormality or the presence of masses, which could lead you to triage the patient to hysteroscopy next rather than biopsy."
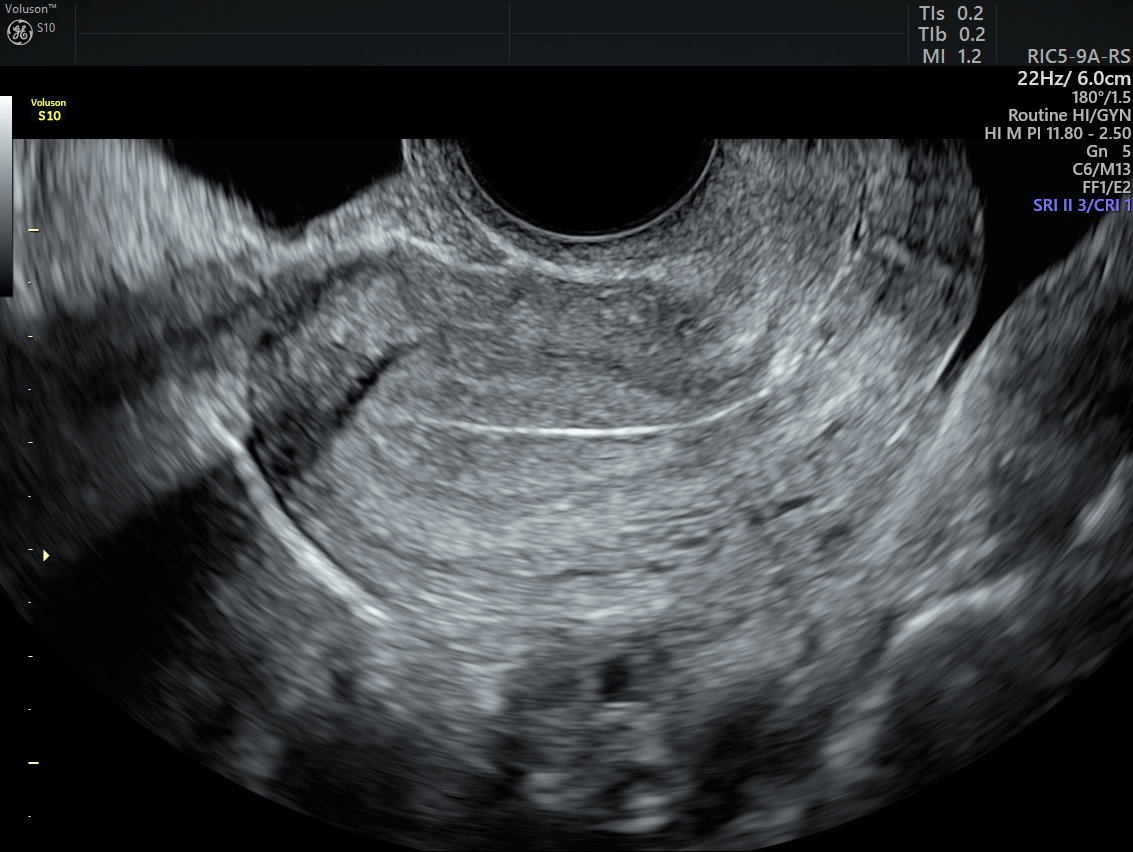
2D ultrasound of thickened endometrium
Dr. Goldstein agrees.
"With ultrasound, I have the ability to reassure [a patient] that she's fine before she even gets to the parking lot," he says. "She knows that she doesn't need any other tests. She doesn't have to go across town to have anything else done. That's important to patients."
Ultrasound vs. Endometrial Sampling
To rule out endometrial hyperplasia, the American College of Obstetricians and Gynecologists (ACOG) suggests ultrasound as a reasonable first-line alternative to endometrial sampling. Specifically, AUB indicates for ultrasound in various contexts, including pelvic ultrasound and saline infusion sonohysterography (SIS), or sonohysterography, per the American Institute of Ultrasound in Medicine. SIS offers a high degree of sensitivity and specificity, and is an effective method in situations where obtaining clear visuals is difficult, such as with obese patients or those who have had previous pelvic surgery or fibroids.
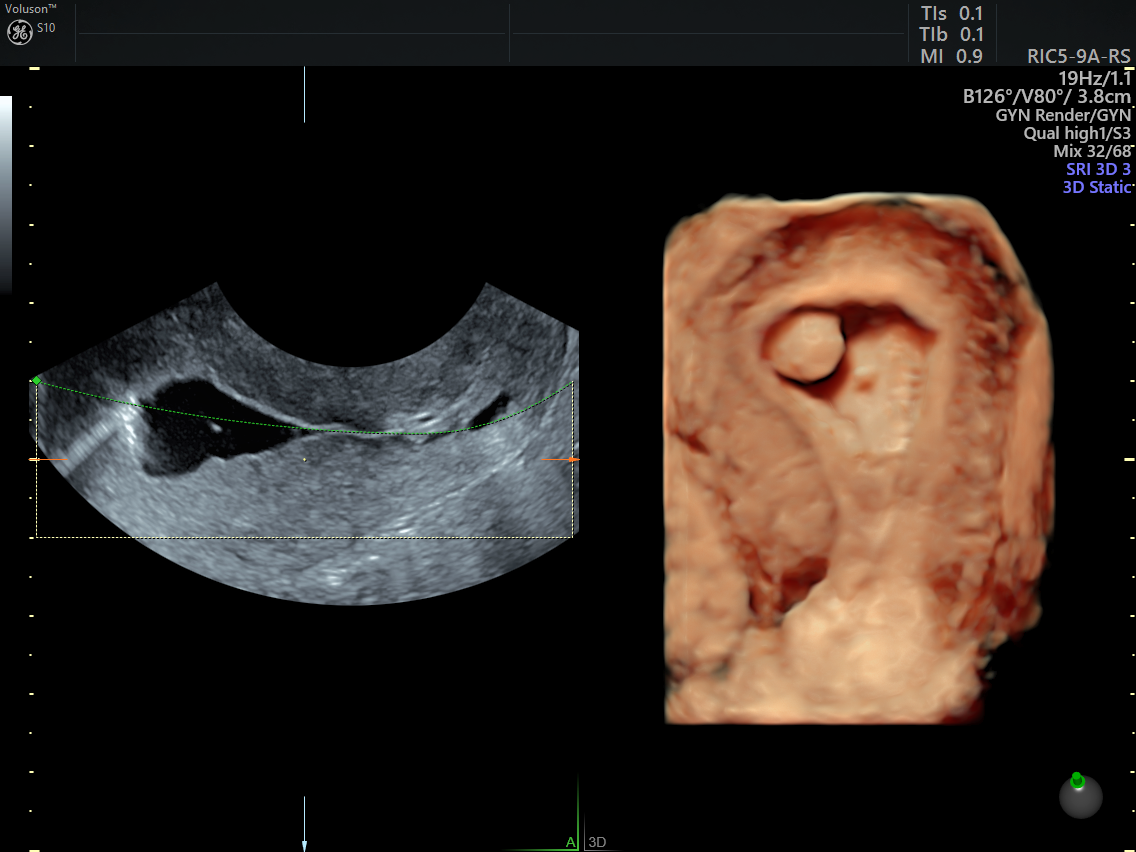
endometrial polyp shown on sonohysterogram
Often,, ultrasound may negate the need for biopsy entirely. One study in the Journal of Obstetrics, Gynecology and Cancer Research found that transvaginal ultrasounds adequately predicted the results of pipelle sampling with a cutoff for endometrial thickness of 10.5 mm. More generally, imaging that reflects a thin, distinct endometrial echo of 4 mm or less can effectively rule out cancer as a possibility.
"It's pretty simple," Dr. Goldstein explains. "The use of ultrasound can virtually always tell you if the patient can be left alone, or if she needs to go to the OR for more intensive diagnostic testing. These women can avoid a dilation and curettage or biopsy and the added cost, discomfort and risk that comes with these procedures."
Given the tendency of blind biopsies to miss potential malignancies, this advantage matters. In one study cited in the Supplement to OBG Management, biopsy samples missed 11 out of 65 known cancers.
"Physicians do a biopsy and think this tiny piece of tissue represents the whole uterus and that's not necessarily true," notes Dr. Goldstein. "Many of these tumors are focal. If you get the wrong wall or the wrong area, you might be misled."
Vaginal Skin Problems
Perimenopausal women commonly report vaginal dryness. But when skin conditions become more concerning — such as frequent vulvar pruritus — it could indicate underlying dermatologic conditions. In those scenarios, ultrasound has clinical utility.
For example, a case report of a 59-year-old woman in Ultrasound in Obstetrics and Gynecology notes the ability of high-frequency ultrasound to determine diagnostic characteristics for vulvar skin conditions, such as size and penetration. Using ultrasound, the providers identified the irregular borders of a targeted skin lesion and were able to diagnose lichen sclerosus.
Abdominal Pain or Extension
Sometimes, transvaginal ultrasounds can help detect malignancies that aren't pathologically uterine, ovarian or endometrial. In a study reported in Ultrasound in Obstetrics and Gynecology, a transvaginal ultrasound ultimately led to a non-Hodgkin lymphoma diagnosis in a patient who reported a distended abdomen. Thanks to that diagnostic clarity, the patient could receive the necessary treatment (chemotherapy).
As the journal notes, such insights help reinforce the need for an "open-minded approach" when it comes to ultrasound. Given the age-related risks of certain hematologic cancers among older patients, gynecologic providers of perimenopausal women cannot afford to overlook ultrasound as an exam option.
UTIs and Incontinence
Though urinary tract infections (UTI) and incontinence are common symptoms of menopausal transition, they may also flag serious conditions like urethral diverticula. When patient cases require more investigation, urogynecological ultrasound can help.
In Ultrasound in Obstetrics and Gynecology, researchers found that transperineal ultrasound clearly represented the patients' urethras well enough to discern abnormalities. Among 23 abnormal reports, physicians identified calcifications, cysts, urethral diverticula and urethrovaginal fistula, demonstrating ultrasound's utility in providing reliable clinical information.
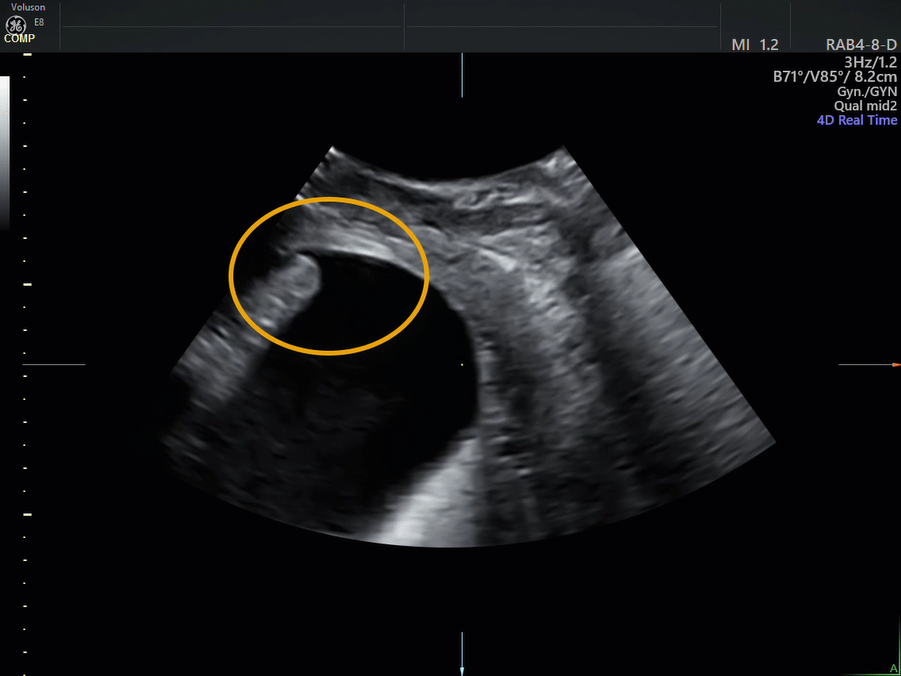
2D ultrasound of urethra
The Intersection of Exceptional Care and Unmatched Experience
Many complaints linked with the perimenopausal transition are just part of this phase. However, in the rare occasion where underlying medical conditions masquerade behind common symptoms, diagnostic tools that quickly detect and assess those issues play a huge role. When those diagnoses can take place noninvasively using ultrasound, it makes for a better overall patient experience that is often easier and more cost-effective than other approaches, such as CT and biopsy.
As the number of people ages 65 and older more than doubles between now and 2050, according to the Population Reference Bureau, the needs of postmenopausal patients will become even more important. The information provided by ultrasound increases physicians' confidence in the diagnosis they are making, enabling them to provide the best care and treatment for this patient population.


