Although they are a relatively rare cause of lower urinary tract symptoms (LUTS), urethral diverticula are increasingly being diagnosed and imaged in-office using ultrasound. The advantages of ultrasound as a diagnostic tool for this often painful condition include its ready availability and noninvasive approach. Additionally, the absence of ionizing radiation and lack of need for contrast make it a safe and cost-effective method that can be used even during pregnancy.
Diagnosing Urethral Diverticula
Standard transducers for transabdominal, transvaginal and transluminal imaging may be used to identify the size, number and location of any vaginal masses that have developed, and the content and wall thickness of the pouch itself. Traditional diagnostic tools such as MRI, urethrecytoscopy, double-balloon catheter urethrography and CT voiding urethrography have confirmed the accuracy of ultrasound results in multiple studies, solidifying its primary role in pinpointing the cause of vexing and often chronic symptoms.
Some disadvantages of ultrasound include dependency on the operator's expertise and misdiagnosis or confusion with paraurethral cysts. Clinicians should take advantage of any training offered by ultrasound manufacturers to keep their skills sharp.
Ultrasound Markers to Look For
On ultrasound, a urethral diverticulum may appear as a cystic, hypoechoic structure below the bladder and urethra. A fluid debris level is often notable. Echogenic debris may be present, and color or power Doppler will reveal an absence of flow. Stones — which are rare, but sometimes form in the urethral diverticula — appear as calcifications in the suburethral area.
When imaging transvaginally, the bladder should not be completely empty so as to better identify pelvic landmarks. A clinician should partially insert the probe, taking care to avoid compressing the urethra. Any compression may distort or obliterate the urethral diverticula.
Transrectal imaging, although often less preferable to patients, sidesteps the issue of urethral compression. The transabdominal and translabial approach may be most acceptable to patients, but due to poor tissue penetration in obese patients, it may be the least sensitive.
Since 3D ultrasound images are easy to obtain, record and transmit, this tool allows for review and consultation with colleagues or specialists without the need for an additional appointment.
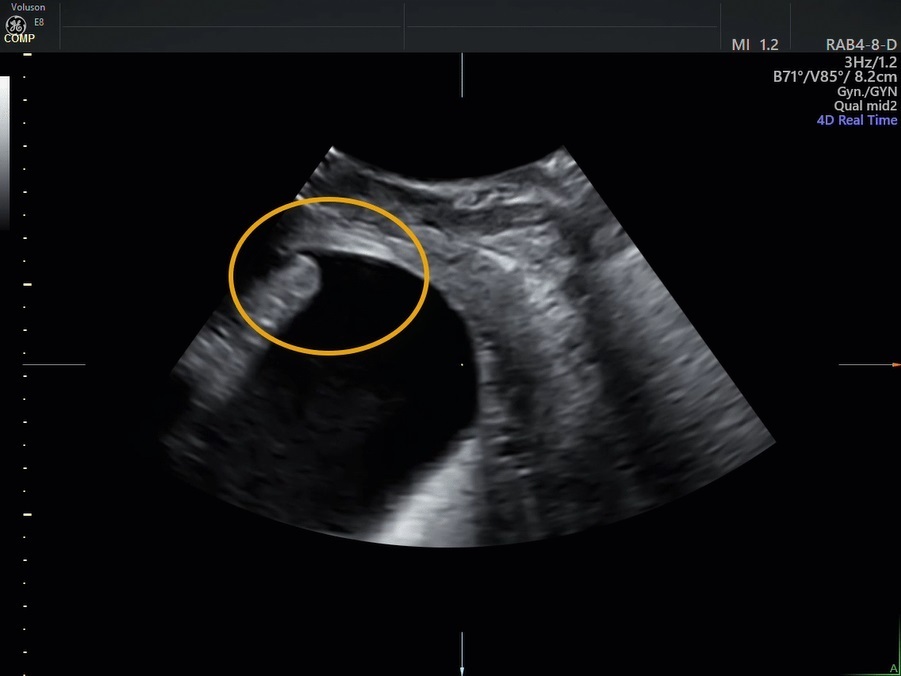
ultrasound image of urethra
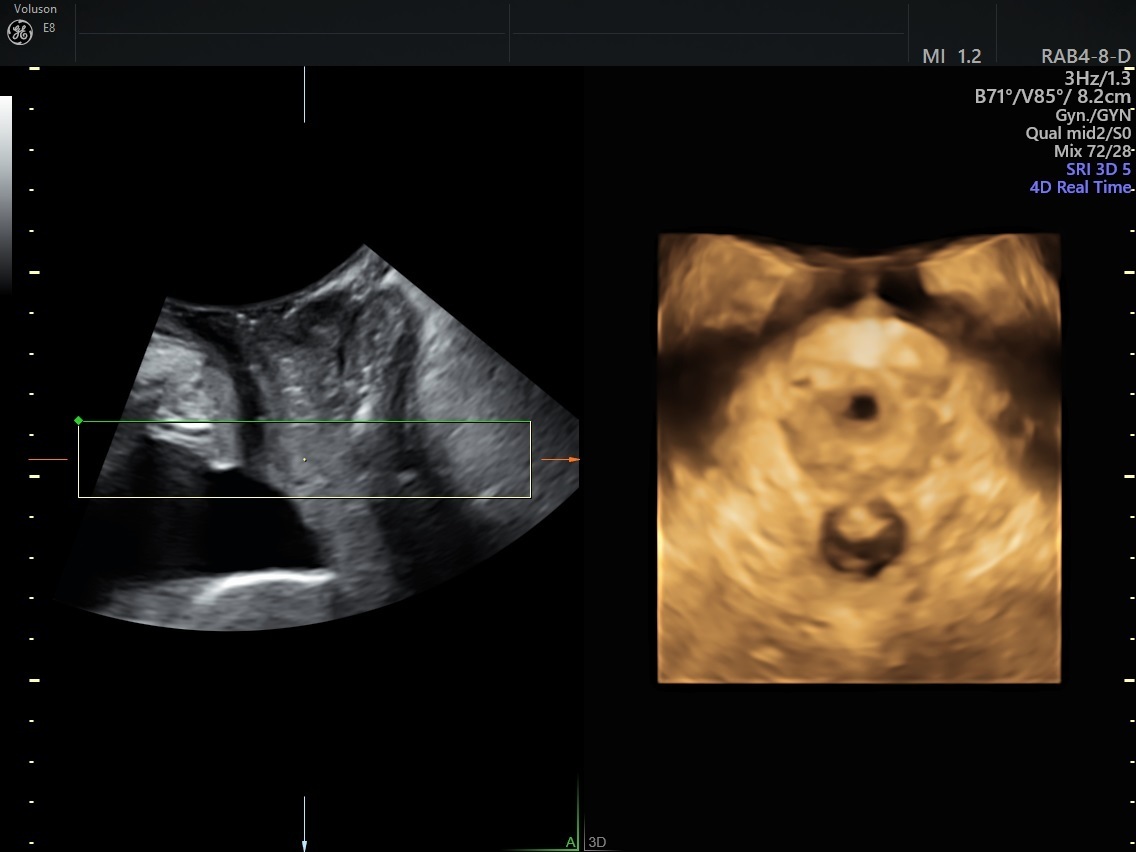
3D ultrasound with volume rendering of normal urethra
Differentiating Between Urethral Diverticula and Similar Conditions
The differential diagnosis includes vaginal wall cysts, Skene's gland abscesses or cysts, ectopic ureteroceles and neoplasms. Both ectopic ureteroceles and cancers of the urethral diverticula are very rare. Ectopic ureteroceles are more commonly diagnosed in children and associated with congenital genitourinary anomalies, such as unilateral duplication of the collection system.
Malignancies of urethral diverticula may be of the adeno, squamous or transitional cell type. Ultrasound features of malignancy include a solid, vascularized mass or an irregular or cystic lesion with thickened irregular walls.
Urethral diverticula can cause a variety of symptoms, although its pathogenesis is not well understood. If a patient presents with a history of chronic urinary tract infections and complaints of chronic vaginal discharge, dysuria and other symptoms of LUTS, clinicians should consider the diagnosis of urethral diverticula. A careful exam and ultrasound will facilitate the diagnosis, and can inform surgical intervention or other treatment that improves the patient's health and quality of life.



