Heart disease and stroke are the leading cause of death in cisgender women, causing 1 in 3 deaths annually — more than all cancers combined. But the majority of those deaths can be prevented, according to the American Heart Association (AHA).
For many women, their OB/GYN is their primary care provider. That means OB/GYNs have a unique opportunity to assess risks and promote prevention. The AHA and the American College of Obstetricians and Gynecologists (ACOG) recommend that OB/GYNs' annual wellness visit guidelines include heart disease risk assessments.
Women's Heart Health and Annual Wellness Exams
Even when women have a primary care provider (PCP), their OB/GYN may be in a position to recognize risk factors not visible to other providers. Research published in the journal Circulation finds that only 45 percent of women and fewer than half of PCPs consider heart disease a top concern. For PCPs, heart disease comes after concerns about breast health and weight.
Plus, the same research notes gender differences in recognizing and addressing heart disease risk factors for cisgender women and cisgender men. Many common risk factors are the same for both populations, but certain factors are even more dangerous for women, such as obesity, smoking, hypertension, diabetes, physical inactivity and high cholesterol. The risks are even higher for transgender women, who have a higher risk of myocardial infarction and death from cardiovascular disease compared to their cisgender peers of the same age, reports research from Reviews in Endocrine and Metabolic Disorders.
AHA and ACOG report that patients with a history of pregnancy complications, including preeclampsia, gestational diabetes, gestational hypertension, preterm delivery and low birth weight, are also at a higher risk of heart issues. Yet adverse pregnancy outcomes are often not part of heart disease risk tools and may not be part of a patient's electronic medical record. That means their PCP, or even cardiologist, may not have full insight into all their risk factors the way their OB/GYN does.
In addition, polycystic ovary syndrome (PCOS), menopausal status, hormone use and functional hypothalamic amenorrhea are risk factors that are not included in current risk assessment tools.
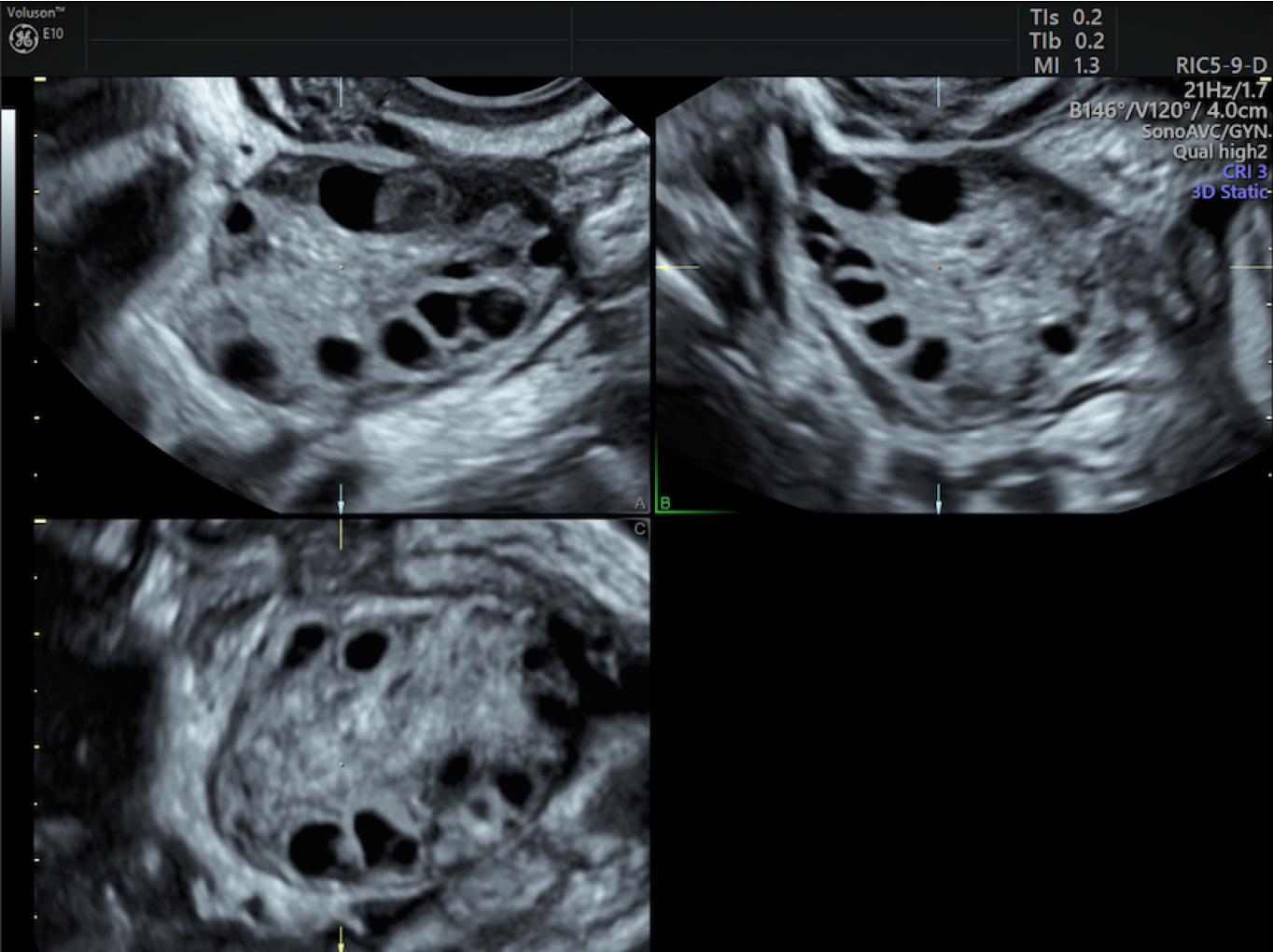
3D Polycystic Ovary is shown using a Voluson™ E10.
Some medical and lifestyle factors do not increase cardiovascular risk individually but do in combination. For example, oral contraceptives alone do not raise the risk of heart disease, but oral contraceptives plus smoking increase the risk seven-fold, according to AHA and ACOG.
Given these gaps in risk assessment, incorporating cardiovascular disease screening into your office's annual wellness visit guidelines can lead OB/GYN patients to life-saving care. Sharing this information with their other specialists can also provide more comprehensive, coordinated care.
How to Incorporate Heart Disease Risk Assessments
OB/GYNs are often busy and have limited time with patients: How can physicians add another assessment to an already packed annual wellness exam? Aim to keep it simple.
- Perform a risk assessment that includes traditional factors as well as pregnancy-related and sex-specific risks.
- Counsel patients on diet, exercise and lifestyle factors that help prevent heart disease, such as quitting smoking, exercising regularly and maintaining a healthy weight.
- Check in on patients' management of chronic conditions, such as high blood pressure, high cholesterol or diabetes. Refer them to a PCP or specialist if they need help managing chronic conditions.
- If a patient has multiple risk factors, refer them to a cardiologist for ongoing monitoring and note relevant risk factors in the referral.
As some patients' primary providers, OB/GYNs are positioned to boost women's heart health. Including some basic screening elements, lifestyle guidance and referrals can ensure patients receive a dedicated, accurate assessment of their heart disease risk.