Copyright© 1988 The American Fertility Society
The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions
The American Fertility Society*
Birmingham, Alabama
The need for standard classification schemes for mechanical problems associated with infertility and fetal wastage is well recognized. In an effort to satisfy this need, The American Fertility Society (AFS) formed a classification committee chaired by Veasy C. Buttram, Jr., M.D. Subcommittees were created to distribute the responsibility for development of the various schemes desired. Committee members were chosen according to their knowledge and desire to contribute. Approval was obtained from the Board of Directors of the AFS and the Executive Committee of The Society of Reproductive Surgeons. Hopefully, editors of medical journals will not accept manuscripts for publication unless they conform to these guidelines. The classification schemes submitted (with a corresponding editorial) are relatively simple to follow. Relevant information can be incorporated into one sheet with appropriate illustrations. In several of the schemes, a scoring system is included to help the surgeon not only document the severity of disease, but to formulate a prognosis. For all schemes a space is provided for the surgeon to note his/her prognosis based upon the extent of pathology and the surgery performed. No classification is perfect, and modification is likely in the future. Use, as well as critique, of these AFS classification is encouraged. All forms, in addition to The Revised-AFS Classification of Endometriosis, will be provided by the AFS administrative office.
Received March 10, 1988. * Drafted by the following committees: Adnexal Adhesions-Editorial: Veasy C. Buttram, Jr., M.D., Committee: Veasy C. Buttram, Jr., M.D., James Daniell, M.D., Richard Dickey, M.D., Victor Gomel, M.D., Jerome Hoffman, M.D., Jaroslav Hulka, M.D., Luigi Mastroianni, Jr., M.D. and Thomas Vaughn, M.D. Distal Tubal Occlusion-Editorial: Victor Gomel, M.D., Committee: Veasy C. Buttram, Jr., M.D., Victor Gomel, M.D. and Carl Levinson, M.D. Tubal Occlusion Secondary to Tubal Ligation-Editorial: Alvin Siegler, M.D., Committee: Veasy C. Buttram, Jr., M.D., Jaroslav Hulka, M.D., Carl Levinson, M.D. and Alvin Siegler, M.D. Tubal Pregnancies-Editorial: Alan DeCherney, M.D., Committee: Veasy C. Buttram, Jr., M.D., Alan DeCherney, M.D. and John Rock, M.D. Mullerian Anomalies-Editorial: William Gibbons, M.D., Committee: Veasy C. Buttram, Jr., M.D., S. Jan Behrman, M.D., Williams Gibbons, M.D., Howard Jones, M.D. and John Rock, M.D. Intrauterine Adhesions-Editorial: Charles March, M.D., Committee: Veasy C. Buttram, Jr., M.D., Alan DeCherney, M.D., Charles March, M.D., Robert Neuwirth, M.D. and Thomas Vaughn, M.D. Reprint requests: The American Fertility Society, 2140 11th Avenue South, Suite 200, Birmingham, Alabama 35205.
Adnexal adhesions
This classification (Table 1) is a modification of the scheme for adnexal adhesions provided in the Revised AFS Classification for Endometriosis.l Although the scores applied to differentiate between minimal, mild, moderate, and severe adhesions are arbitrary, they are considered appropriate until prospective studies are performed that dictate the need for change. Important features of this scheme are that (1) the prognosis for conception is based on the score applied for the adnexa with the least amount of pathology, (2) the importance of the fimbriated end
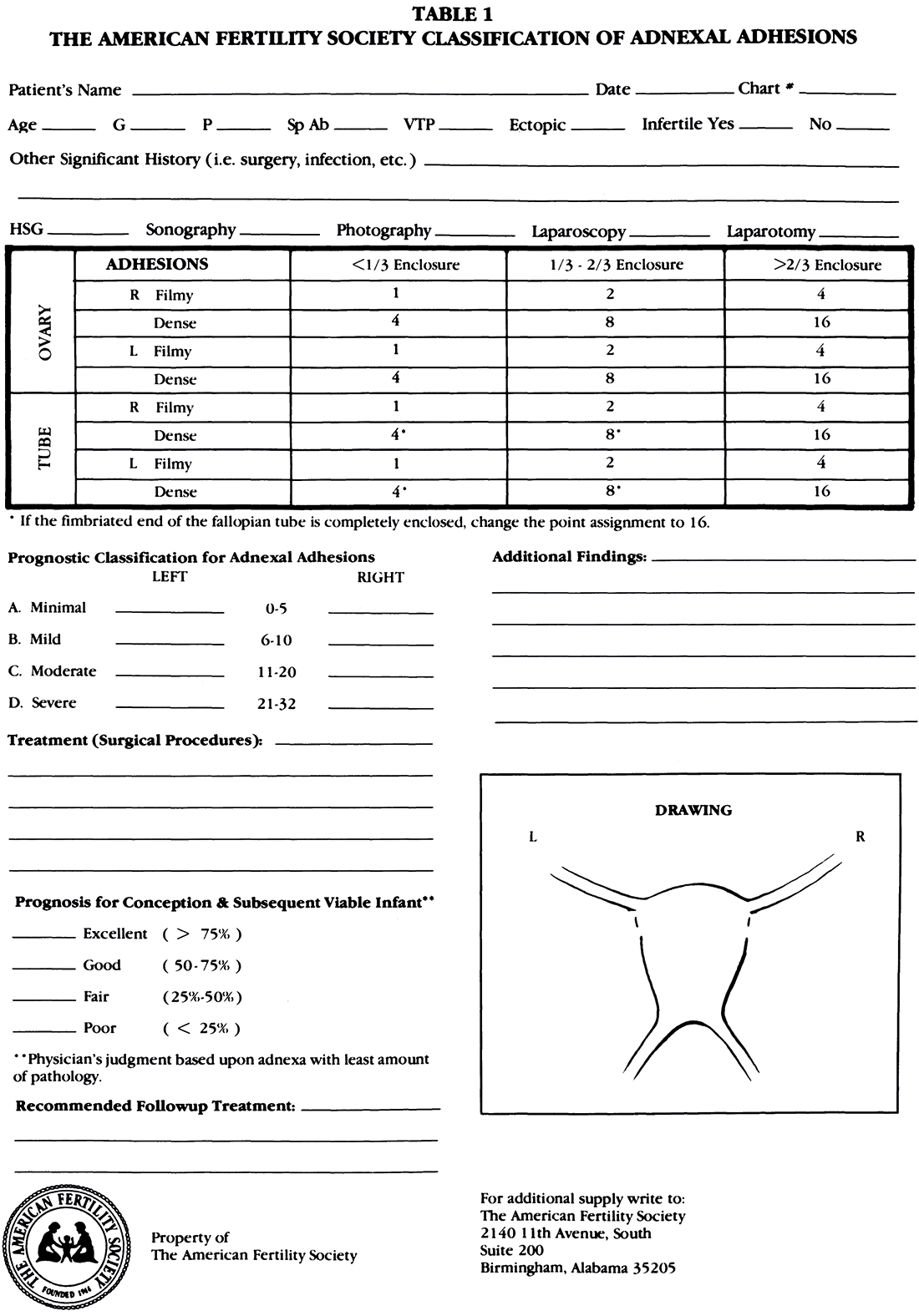
of the fallopian tube is emphasized, and (3) a differentiation is made between filmy and dense adhesions. The latter subjective observation may create conflict among gynecologists. However, it is the responsibility of the physician to make judgment not only of the extent of the disease, but a distinction between what are thought to be filmy and dense adhesions. Generally, filmy adhesions can be lysed by scissors, electrocautery, or laser without undue risk of bleeding or injury to adjacent organs.
Distal tubal occlusion
Salpingostomy (salpingoneostomy) is the creation
of a tubal ostium in a tube with a totally
occluded fimbriated end as is found in a hydrosalpinx
or sactosalpinx.2
The Ad Hoc Committee of the International
Federation of Fertility and Sterility (IFFS) classified
salpingostomy (salpingoneostomy) as (a) terminal,
(b) ampullary, and (c) isthmic.3,4 A terminal
salpingostomy is preferable since the tube is conserved
in its entirely and normal tubo-ovarian relationships
are maintained. Specific circumstances
such as the presence of extensive intratubal adhesions
in the terminal portion of the tube may oblige
the surgeon to excise the affected portion of the
oviduct and resort to an ampullary salpingostomy.
Reversal of a prior fimbriectomy (Koerner's sterilization)
also requires an ampullary salpingostomy;
this is outside the scope of this editorial, which is
limited to distal occlusion caused by pelvic inflammatory
disease. Isthmic salpingostomies have an
exceedingly poor yield and should be abandoned.
The utilization of microsurgical techniques in
reconstructive infertility surgery has yielded significant
improvements in the results of these procedures.
However, improvements in outcome have
not been as evident in salpingostomy for hydrosalpinx
despite the high postoperative tubal patency
rate obtained with microsurgery. The relative improvement
in the rate of intrauterine pregnancy
noted after such procedures may be due to the increase
in the rate of postoperative patency, which
in turn is also responsible for the significant rise in
the rate of tubal pregnancy. The surgery-pregnancy
time interval after salpingostomy is fairly
long; more than 60% of the patients who achieved
an intrauterine pregnancy did so after the first
postoperative year.5-9
Tubal function, hence the pregnancy rate subsequent
to a salpingostomy for hydrosalpinx, is
largely dependent on the status of the fallopian
tube at the time of the surgical intervention. Individually
and collectively, the following factors affect
the outcome: condition of the endosalpinx, extent
of ampullary dilatation, thickness and rigidity
of the tubal wall, extent and nature of pelvic and
periadnexal adhesions.10 The presence of well-defined
regal markings within the oviduct, especially
when not greatly dilated indicates a good prognosis11
Conversely, intratubal adhesions, especially
when they involve a large part of the oviduct,
represent a contraindication to salpingostomy.12
The prognosis is affected adversely by the extent of
ampullary dilatation, especially if this is more than
3 cmY-15 A hydrosalpinx with rigid, thickened
tubal wall carries an exceedingly poor prognosis.
These tubes show little evidence of dilatation.12,16,17
In addition, the prognosis is inversely proportional
to the extent ofthe periadnexal and pelvic adhesive
process.12-14,16
The tools currently available to investigate the
oviducts are hysterosalpingography and laparoscopy.
They are complementary procedures, and
they are more effective in identifying cases at the
extremes of the spectrum. At one extreme are the
favorable cases, with tubes that show little dilatation,
exhibit rugal markings, are supple without
any suggestion of tubal wall thickening, and without
significant pelvic or periadnexal adhesions. At
the other extreme, the findings are sufficiently severe
to conclude that surgery is contraindicated;
these include the presence of extensive, dense pelvic
adhesions; extensive intratubal adhesions; extreme
dilatation of the tubes; or changes consistent
with or evidence of prior tuberculous salgingitis.
The intermediate cases may be more difficult to
assess. In certain instances periadnexal adhesions
prevent proper visualization and assessment of the
oviduct. Frequently, it is difficult to assess accurately
the thickness and rigidity of the tubal wall
until the time of the actual surgery. The value of
salpingoscopy (performed during the diagnostic
laparoscopy) in predicting postoperative prognosis
is currently under investigation.
The reported viable pregnancy rates subsequent
to microsurgical salpingostomy vary between 19%
and 35%, and the ectopic pregnancy rate ranges
between 5% and 18%. Both intrauterine and ectopic
pregnancy rates increase with longer followup
periods. With favorable cases the outcome is
better; intrauterine pregnancy rates varying between
50% and 80% have been reported.13,16-18 For
this reason, several authors have proposed a scoring
system to identify prognostically favorable
cases. Owing to the progress in the field of in vitro
fertilization, this therapeutic modality has become
a credible alternative to surgery in cases of hydrosalpinx.
This development argues in favor of a
more rigorous selection of patients for microsurgical
treatment. Furthermore, in selected cases laparoscopic
salpingostomy provides another alternative
to microsurgery; this has the advantage of
being performed during the initial diagnostic laparoscopy
without recourse to a laparotomy.19-21 A
better understanding of the prognostic factors will
permit the selection of the most appropriate treatment
modality; this individualization of therapy
should enable us to achieve better overall results.
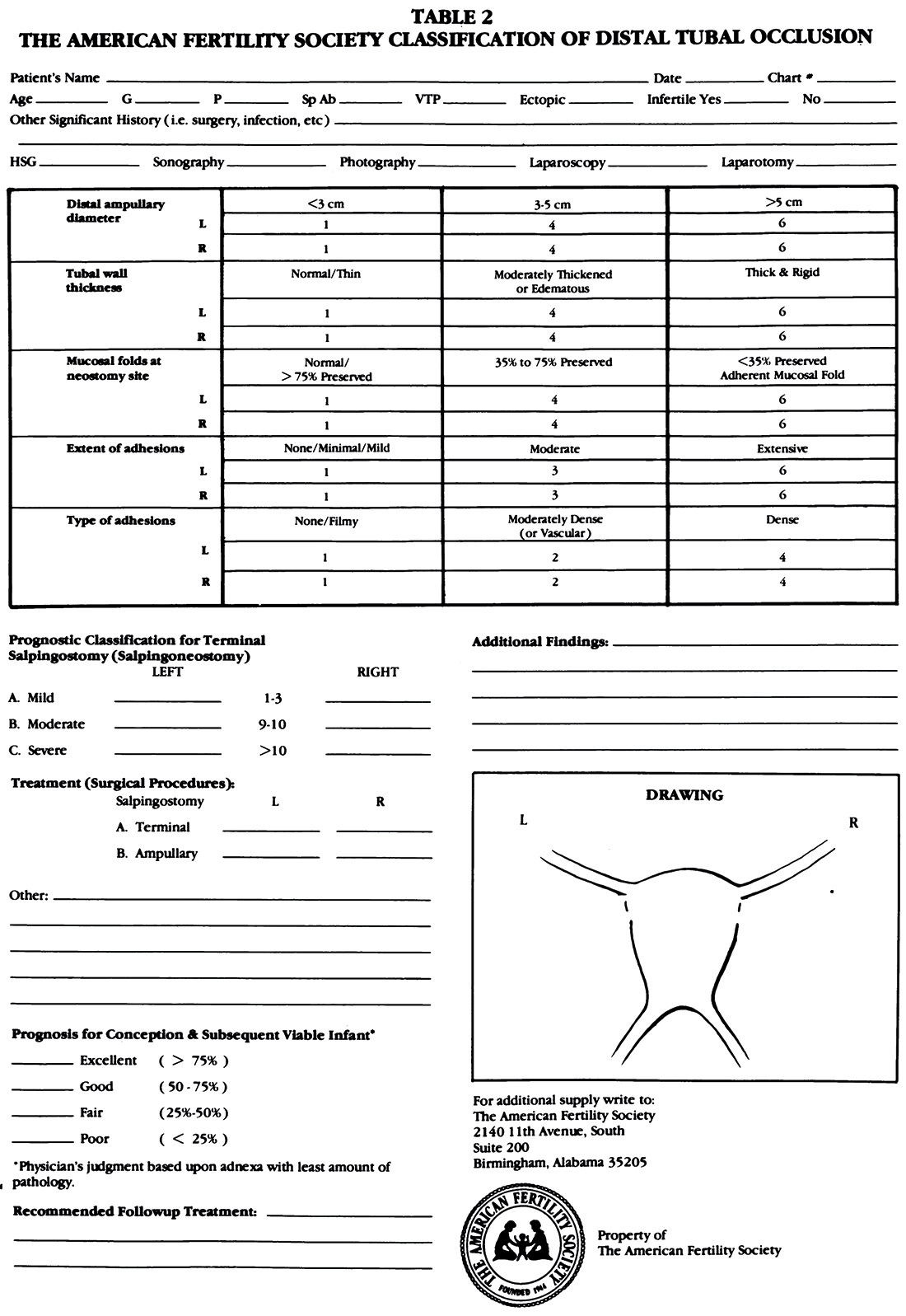
The proposed scoring system (Table 2) has been
devised to predict the postoperative prognosis of
salpingostomies whether performed by laparotomy
or laparoscopy. It has been designed for use at the
time of the actual reconstructive surgery but may
also be employed at the completion of the preoperative
investigation to determine the accuracy of the
information gained. Various factors known to affect
the prognosis have been assigned values. Although
the assignment of specific numbers may
appear arbitrary, they have been selected after
taking into account observations and conclusions
of the previously cited reports. The factors to be
scored include extent and nature (type) of adhesions,
thickness and rigidity of the tubal wall, the
distal ampullary diameter, and the extent of preservation
of mucosal folds in the neostomy site. We
recommend the use of the IFFS classification to
quantify the extent of adhesions, since one already
exists. Minimal/mild: 1 cm of tube and/or ovary
involved. Moderate: adhesions partially surround
tube and/or ovary. Extensive: peritubal and periovarian
adhesions totally encapsulate the tube
and/or ovary. Along with other investigators,22 we
recommend intraoperative salpingoscopy to visualize
the whole length of the ampullary lumen.
Whereas the status of the ampullary endosalpinx is
also an important prognostic parameter, we elected
not to include it in the scoring system at this time,
since salpingoscopy is not being practiced universally.
The proposed classification and the various
values (numbers) in the scoring system will need to
be modified as a result of prospective studies. This
task was undertaken without any illusion that it
would yield the perfect classification; however, a
beginning was necessary.
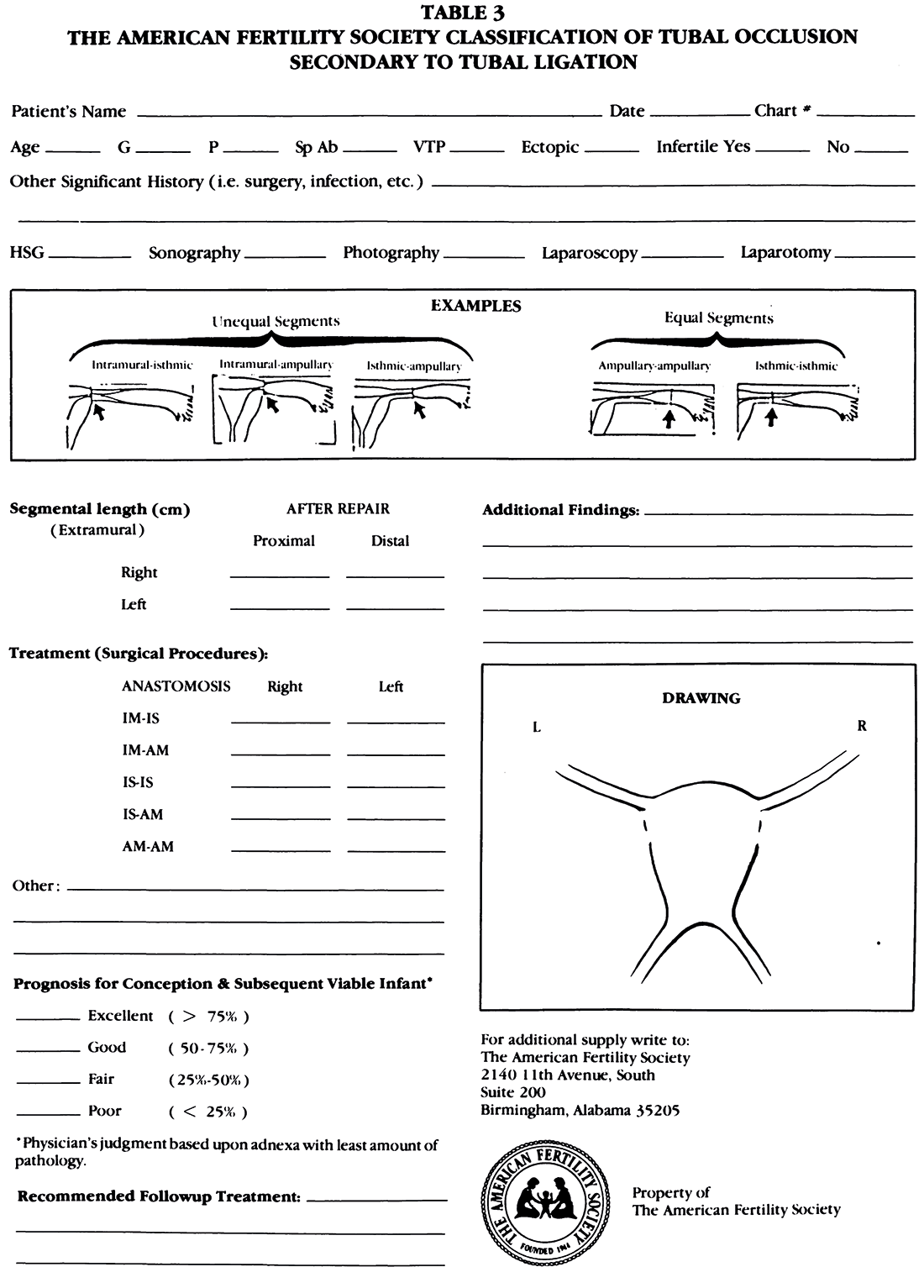
Tubal occlusion secondary to tubal ligation
The purpose of this operative classification
(Table 3) is to be able to dentify similar procedures
so that reasonable comparisons can be made
among different studies, prognoses can be given to
patients who then make informed choices, and
physicians can respond to their queries with increased
knowledge.
The type of sterilization can influence the technique
of repair and prognosis. The influence of age
on success is likely. Older women usually have
longer intervals since sterilization, increased ovulatory
disturbances, and older partners. Thus, not
only age but time interval from sterilization to reversal
is important to document. Electron microscopic
studies have shown relative atrophy of the
tubal epithelium in the proximal stumps of women
sterilized more than 5 years prior to reversals and
increased abnormalities between the sterilization
and sterilization reversal (SR). These include flattening
of mucosal folds, deciliation, adenomyosis,
and polyposis. Disorders of the tubal isthmus occur
with chronic (long-standing) occlusion. It is important
to perform a hysterosalpingogram (HSG)
prior to surgery to determine the status of the
proximal portion of the fallopian tubes. Although
laparoscopy is not essential when one is confident
regarding the status of the distal portion of the
fallopian tubes, it is generally advisable.
The lengths of the tubes after completion of the
SR operation should be recorded. The types of
anastomoses are intramural-isthmic, intramuralampullary,
isthmic-isthmic, isthmic-ampullary,
and ampullary-ampullary. Equal-sized lumens
represent either isthmic-isthmic or ampullaryampullary
anastomoses. It is uncommon to encounter
significant periadnexal adhesions in these
women during the SR, and it is not necessary to
add a point scoring system for adhesions. The performance
of other tubal or pelvic procedures and
associated abnormalities should be listed.
Few series of more than 50 SRs have been reported;
postoperatively the live births vary from
48% to 78% and the tubal pregnancies from 1.7% to
6.5%. Since there are an estimated 5,000 reversal
procedures performed annually and less than 1,000
have been reported, it is obvious that most SRs are
being done by the "Silent Majority."
Operations for reversals, other than anastomosis,
include salpingoneostomy and utero-tubal implantation,
the latter involving either the isthmus
or ampulla. The length of the extrauterine portion
of tubal segment should be measured as well as its
new location in the uterine wall. Salpingoneostomy
is done for reversal of a previous fimbriectomy, and
the length of the extrauterine tubal segment should
be noted. Laparoscopy is essential in these patients
before SR is attempted.
A separate classification is needed for anastomosis
operations performed because of pathologic
rather than iatrogenic occlusions. These procedures
have a different prognosis from those done
for SR. Invariably, these women will need a
screening HSG and laparoscopy; however, the categories
for anastomosis are quite similar to those for
SR. We would suggest including a category entitled
"Surgical Pathology Report." The listings would be
luminal fibrosis, salpingitis isthmica nodosa, endometriosis,
tuberculosis, and other. Of concern is
that in approximately 10% of specimens for histologic
examination, no pathologic lesions are found.
Tubal pregnancies
Approximately 60,000 ectopic pregnancies occur
in this country in a single chronologic year, making
surgery for an ectopic pregnancy a frequently performed
procedure in reproductive surgery.
New technology has changed ectopic pregnancy
as an entity, both in diagnosis and in management.
The combination of serial beta pregnancy testing
and ultrasound, both abdominal and vaginal, has
increased our diagnostic acuity so that ectopic
pregnancies are now diagnosed between 6 and 8
weeks gestation, instead of being diagnosed at 10
weeks or later as in the past. This change has
ushered in the age of conservative surgery in the
management of ectopic pregnancy, in contradistinction
to the ablative surgery that was done a
decade ago. At that time, ectopic pregnancies were
diagnosed after rupture has occurred, and very little
in the way of alternative remained.
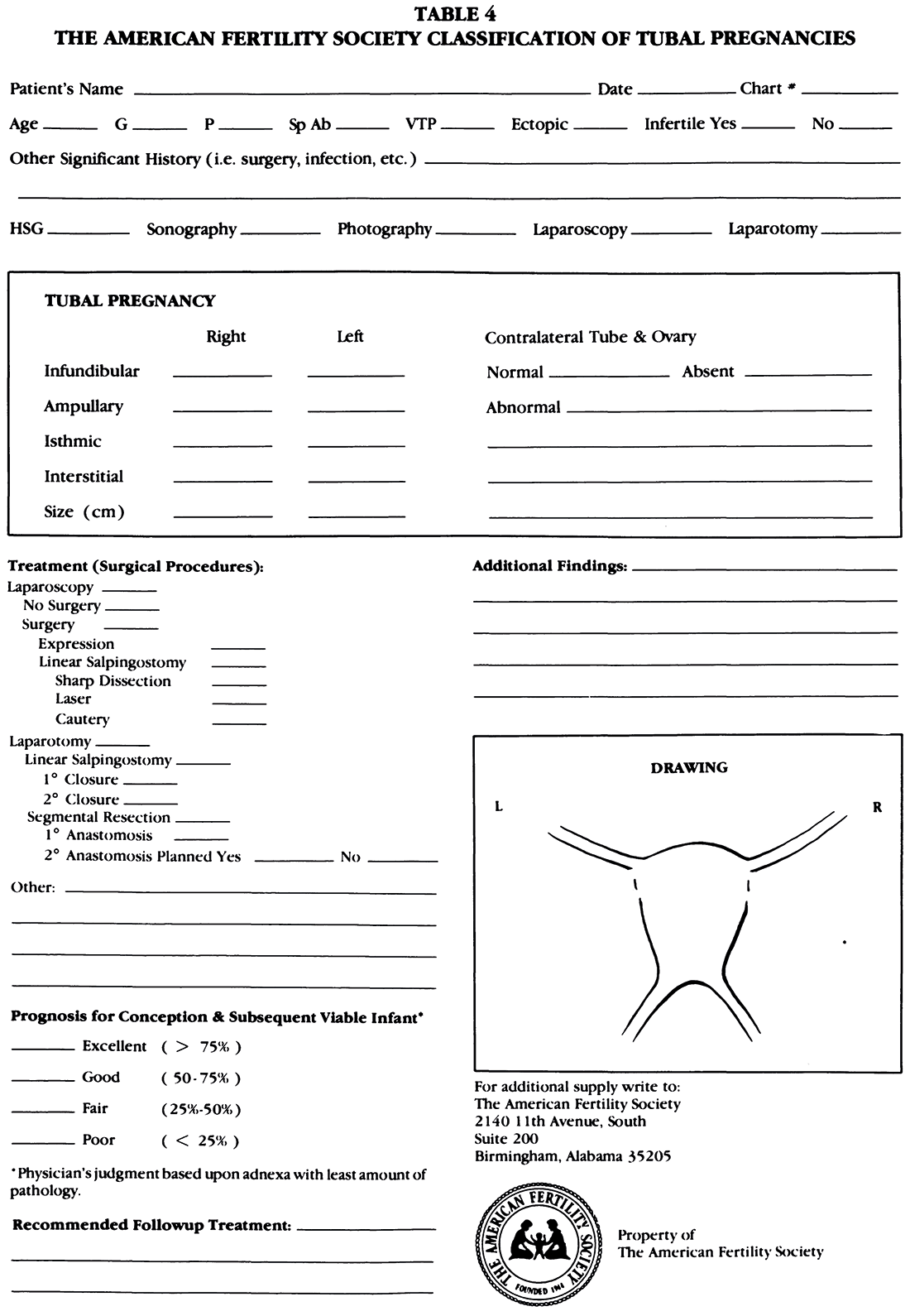
Classification for ectopic pregnancy should be
comprehensive, and not overwhelming. It should be
helpful and informative. Completion of the forms
should be a welcome addition to management,
rather than a chore. This classification of ectopic
pregnancy (Table 4) includes some historic facts
indigenous to the patient that indicate a high risk
for ectopic pregnancy, i.e., previous tubal surgery,
previous ectopic pregnancy.
The anatomic location of the ectopic pregnancy
is critical. Ampullary ectopic pregnancies usually
grow outside of the lumen, and therefore postoperative
patency is to be expected. Linear salpingostomy
seems to be the treatment of choice in these
cases. Conversely, isthmic ectopic pregnancies
grow within the lumen and destroy the tubal mucosa;
in these cases, segmental resection seems to
be the treatment of choice.23 Interstitial pregnancies
in time will most likely be treated by chemotherapy,
not surgery; therefore, this is also important
to note. Ruptured or unruptured should be
noted, and site of rupture, or imminent rupture are
also critical issues since ectopics that rupture into
the broad ligament, rather than dorsally, represent
an entirely distinct entity requiring more extensive
surgery.
It is essential to record the mode of treatment.
Many ectopic pregnancies are now removed by a
laparoscopic approach as opposed to laparoscopic
diagnosis with treatment at laparotomy. The
method of surgical repair should also be included:
magnification vs. no magnification. The method
of surgical approach needs to be elucidated (no
surgery, expression [milking the tube], linear
salpingostomy, or segmental resection with primary
or secondary anastomosis or no anastomosis
planned). Also to be considered in the classification
are other anatomic observations including adhesions,
status of the contralateral tube, and corpus
luteum. And last, adjunctive therapy and postoperative
course are helpful.
In any classification, foresight is the key. What
will you want to know in the future about this particular
patient? This information is critical in
counseling patients about future success rates,
especially now that patients are having multiple
ectopic pregnancies, rather than only two as in the
past.24
Mullerian anomalies
The reason for providing a standardized classification is its value to the practicing physician. It should be simple to use to promote compliance and flexible enough to provide the capacity to fit almost "every" possibility. A frequently used classification by Strassman25 grouped the anomalies into the symmetric double malformations (didelphus, bicornuate, septate) or the asymmetric ones (unicornuate with or without a rudimentary horn). This resulted in a reduction in the amount of available information that reached the literature because of arbitrary groupings particularly with regard to the bicornuate and septate uteri. Consequently, if the clinician wishes to inform, for example, a patient with a unicornuate uterus with a
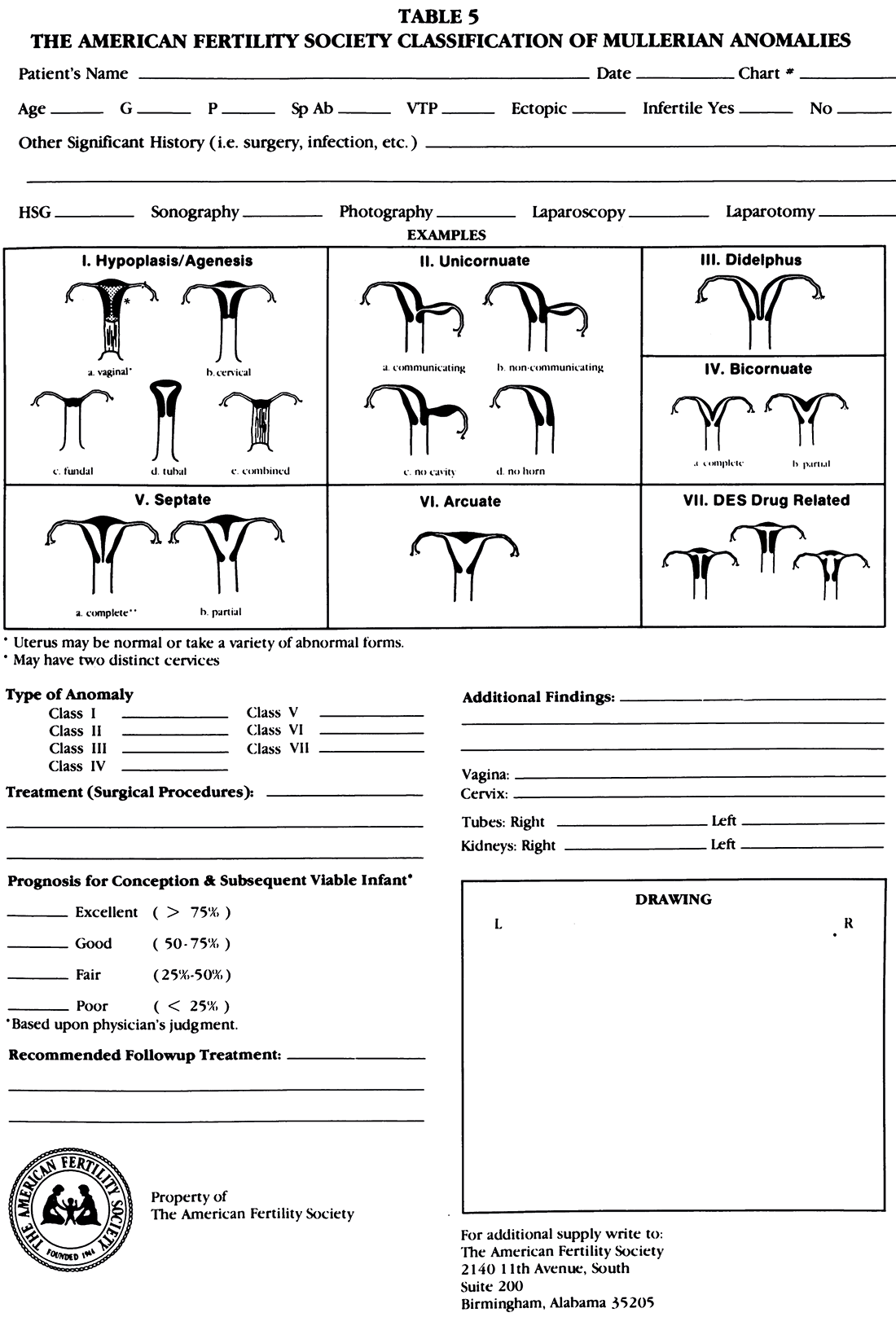
rudimentary functional horn of her prognosis, the sources are limited to individual case reports or a single series containing few cases. Few reports in the literature provide fetal wastage rates for separate uterine malformations.26-29 The conclusions reached in these individual series vary greatly because they are based on such a small number of observations. An easy-to-use flexible reporting system will allow the clinician to group cases with others so that in the future appropriate conclusions can be reached based on adequate numbers. This classification (Table 5) organizes the anomalies according to the major uterine anatomic types. It allows the user to indicate the malformation type as well as the associated variations involving the vagina, cervix, tubes, ovaries, and urologic system. Later, when data is compiled, a unique "computerizable" code can be generated for reporting purposes. The classification committee had difficulty deciding how to include the arcuate uterus. Because the arcuate uterus is externally unified, it could be classified as a form of a partial septate uterus. However, since in contrast to the other malformations, the arcuate uterus appears to behave benignly, it was thought that it should be classified separately for the present. Thus, data can be generated that can be used to determine if it should remain in a classification of abnormal uterine malformations or is a variant of normal anatomy.
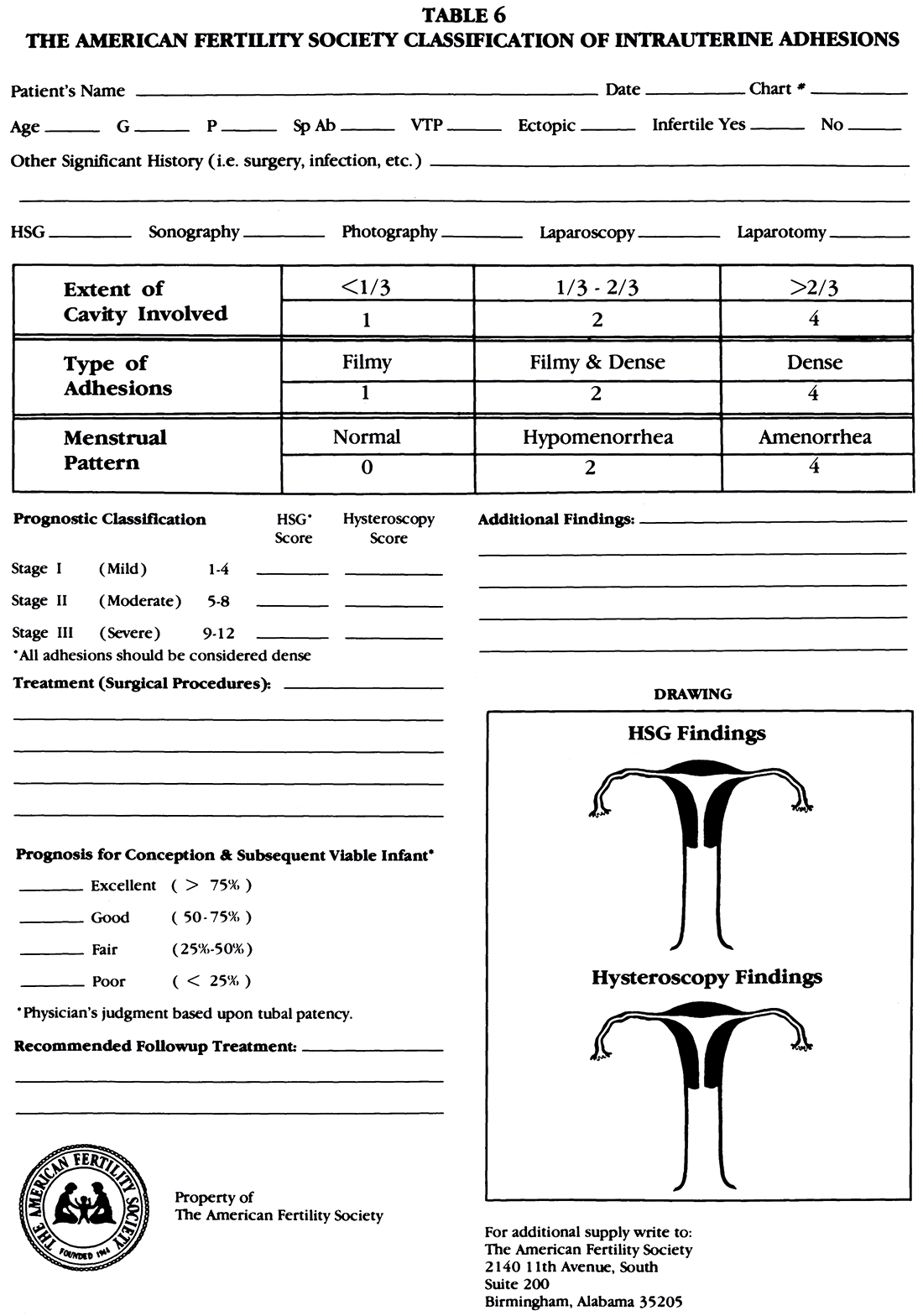
Intrauterine adhesions
The charge to our committee was to develop a
simple classification system for intrauterine adhesions
(IVA). Although other schema to grade IVA
have been available, the widespread use of hysteroscopy
demonstrated their flaws. The first endoscopic
classification was accurate but failed to consider
menstrual pattern, thus the prognostic significance
of endometrial sclerosis or atropy could not
be considered.30
The classification proposed (Table 6) provides
an objective scoring system that permits both the
indirect (hysterographic) and direct (hysteroscopic)
grading of IVA. The location of adhesions is
likely to be of prognostic importance for infertile
women because most implantations occur in the
top-fundal portion of the uterus and because adhesions
in the cornual recesses may cause tubal obstruction.
Drawings should be made to document
location and extent of adhesions. Thus, these findings,
as well as those of laparoscopy should be recorded in the
section entitled "Additional Findings."
The number of classifications of IVA is exceeded
only by the number of treatment regimens. Because
suitable intrauterine contraceptive devices
are no longer readily available to use as "splints"
within the uterine cavity, many treatment schemes
are likely to change. Therefore, these data are even
more important.
Finally, it is advised that one classification form
be completed immediately after surgery and another
following all therapy including the follow-up
hysterosalpingogram or hysteroscopy that is performed
before permitting the patient to attempt
pregnancy. The comparison of the two forms will
provide objective data about the success of therapy
and will permit the true worth of the classification
system to be assessed.
As with the classification system for endometriosis,
continuous evolution is expected. The comparison
with an earlier successful classification reported
in this journal attests to the workability of
the new system. However, broader application may
cause flaws to become more evident resulting in
additions, deletions and/or modifications.
References
1. The American Fertility Society: Revised classification of
endometriosis. Fertil Steril 43:351, 1985
2. Gomel V: Correction of terminal occlusion ofthe oviduct. In
Microsurgery in Female Infertility, Boston, Little, Brown
and Company, 1983, p 163
3. Gomel V: Recent advances in surgical correction of tubal
diseases producing infertility. Curr Probl Obstet Gynecol
1:10, 1978
4. Gomel V: Classification of operations for tubal and peritoneal
factors causing infertility. Clin Obstet GynecoI23:1259,
1980
5. Gomel V: Salpingstomy by microsurgery. Fertil Steril
29:380, 1978
6. Gomel V, Swolin K: Salpingostomy: microsurgical technique
and results. Clin Obstet Gynecol 23:1243, 1980
7. Jansen RPS: Surgery-pregnancy time intervals after salpingolysis,
unilateral salpingostomy, and bilateral salpingostomy.
Fertil Steril 34:222, 1980
8. Russell JB, DeCherney AH, Laufer N, Polan ML, Naftolin
F: Neosalpingostomy: comparison of 24- and 72-month follow-
up time shows increased pregnancy rate. Fertil Steril
45:296, 1986
9. Kitchin JD III, Nunley WC Jr, Bateman BG: Surgical management
of distal tubal occlusion. Am J Obstet Gynecol
155:524, 1986
10. Gomel V: Results of reconstructive infertility surgery. In
Microsurgery in Female Infertility, Boston, Little, Brown
and Company, 1983, p 225
11. Ozaras H: The value of plastic operations on the fallopian
tubes in the treatment of female infertility: a clinical and
radiologic study. Acta Obstet Gynecol Scand 47:489,1968
12. Gomel V: Contraindications. In Microsurgery in Female Infertility,
Boston, Little, Brown and Company, 1983, p 129
13. Rock JA, Katayama P, Martin EJ, Woodruff JD, Jones HW
Jr: Factors influencing the success of salpingostomy techniques
for distal fimbrial obstruction. Obstet Gynecol
52:591, 1978
14. Verhoeven HC, Berry H, Frantzen C, Schlosser HW: Surgical
treatment for distal tubal occlusion: a review of 167
cases. J Reprod Med 28:293, 1983
15. Donnez J, Casanas-Roux F: Prognostic factors of fimbrial
microsurgery. Fertil Steril 46:200, 1986
16. Boer-Meisel ME, te Velde ER, Habbema JDF, Kardaun
JWPF: Predicting the pregnancy outcome in patients
treated for hydrosalpinx: a prospective study. Fertil Steril
45:23,1986
17. Mage G, Pouly JL, de Joliniere JB, Chabrand S, Riouallon
A, Bruhat M-A: A preoperative classification to predict the
intrauterine and ectopic pregnancy rates after distal tubal
microsurgery. Fertil Steril46:807, 1986
18. Frantzen G, Schlosser HW: Microsurgery and postinfectious
tubal infertility. Fertil Steril 38:397, 1982
19. Gomel V: Salpingostomy by laparoscopy. J Reprod Med
18:265, 1977
20. Gomel V, Taylor PJ, Yuzpe AA, Rioux JE: Laparoscopy and
Hysteroscopy in Gynecologic Practice. Chicago, Year Book
Medical Publishers, Inc, 1986, p 148
21. Daniell JF, Herbert CM: Laparoscopic salpingostomy utilizing
the CO2 laser. Fertil Steril 41:558, 1984
22. Henry-Suchet J, Loffredo V, Tesquier L, Pez JP: Endoscopy
of the tube (tuboscopy): its prognostic value for tuboplasties.
Acta Eur Fertil16:139, 1985
23. DeCherney AH, Maheuz R: Modern management of ectopic
pregnancy. Curr Prob Obstet Gynecol, Chicago, Year Book
Medical Publishers, 6:9, 1983
24. Silidker J, Tarlatzis BC, DeCherney AH: Fecundite apres
deux grossesses ectopique. Contraception-Fertilite-Sexualite
12:701, 1984
25. Strassman P: Die operative vereinigung eines doppelten
uterus. Zentralbl Gynakol 31:1322, 1907
26. Caprara BJ, Chuang JT, Randall CL: Improved fetal salvage
after metroplasty. Obstet Gyneco131:97, 1968
27. Michalas S, Prebedourakis C, Lolis D, Antasalkis A: Effect
of congenital uterine abnormalities on pregnancy. Int Surg
61:557, 1976
28. Behrman SJ, Musich JR: Obstetrical outcome before and
after metroplasty in women with uterine anomalies. Obstet
Gynecol 52:63, 1978
29. Buttram VC Jr, Gibbons WE: Mullerian anomalies: a proposed
classification (an analysis of 144 cases). Fertil Steril
32:40,1979
30. March CM, Israel R, March AD: Hysteroscopic management
of intrauterine adhesions. Am J Obstet Gynecol
130:653, 1978
